
Gallstones
Gallstones
Last Section Update: 06/2018
Contributor(s): Maureen Williams, ND; Shayna Sandhaus, PhD
1 Overview
Summary and Quick Facts for Gallstones
- Gallstones are hard deposits of bile components that form in the gallbladder or bile ducts. As many as 80% of gallstone cases are silent, causing no immediate signs or symptoms.
- In this protocol you will learn how gallstones form and are diagnosed, the available conventional treatment options, and surgical approaches that are continually being refined. You will also learn about diet, lifestyle and integrative approaches to reducing the risk of gallstones and their complications.
- Dietary, lifestyle and natural medicine interventions may help people with silent gallstones avoid progressing to a symptomatic stage of gallstone disease. For all forms of symptomatic gallstone disease, surgery is the mainstay of conventional treatment.
What are Gallstones?
Gallstones are hard deposits formed from bile components in the gallbladder or bile ducts. Gallstones are most commonly formed when there is an excess of cholesterol in the bile, causing it to crystallize. Blockages caused by gallstones can cause moderate to severe pain, and can lead to several complications, including inflammation of the gallbladder and infection of the bile ducts. Gallstones are also linked to increased risk of certain cancers and cardiovascular diseases.
For many, gallstone formation is linked with a typical western diet consisting of high amounts of cholesterol and saturated fats.
Natural integrative interventions like vitamin C and omega-3 fatty acids may help reduce the risk of gallstone formation.
What Increases Gallstone Risk?
- A western diet high in saturated fats and cholesterol and low in fiber is one of the strongest risk factors.
- Age
- Gender – women are more likely than men to develop cholesterol gallstones.
- Ethnicity – native North and South Americans and Mexican Americans have a higher risk.
- Genetic predisposition
- Obesity
- Rapid weight loss, prolonged fasting, and weight cycling
- Total parenteral nutrition (TPN, ie, all nutrition is derived intravenously)
- Medications including female hormones and thiazide diuretics (mainly used to treat high blood pressure)
- Sedentary lifestyle
- Other diseases and conditions such as metabolic syndrome, celiac disease, and some liver diseases
What are the Signs and Symptoms of Gallstones?
- Biliary pain (acute, severe pain in the upper-right or upper-mid region of the abdomen)
- Biliary pain that lasts more than 24 hours and is accompanied by nausea, fever, or jaundice can indicate a complication associated with gallstones and warrants emergent evaluation.
What are the Conventional Medical Treatments for Gallstones?
- Gallbladder removal (cholecystectomy)
- Ursodeoxycholic acid may be an alternative to surgery for small, cholesterol-rich gallstones, but can take years to completely dissolve them.
- Other interventions including combination procedures to remove stones from the common bile duct, stone fragmentation, and balloon dilation of the bile duct opening.
What Novel and Emerging Therapies Appear Promising for Gallstones?
- The anti-diabetes medication metformin
- Cholesterol-lowering medications such as statins and ezetimibe (Zetia)
- Surgical advances, including natural orifice transluminal endoscopic surgery (NOTES)
What Dietary and Lifestyle Changes Can Help Relieve Gallstones?
- A diet rich in fiber, plant proteins, fruits and vegetables, and mono- and polyunsaturated fats can protect against gallstone formation.
- Weight loss reduces the risk of gallstones in obese individuals, but rapid weight loss can increase the risk. Someone who wishes to lose weight to decrease the risk of gallstones should try to control their rate of weight loss by modestly restricting calories and keeping a small amount of fat in their diet.
- The addition of certain foods, including coffee, tea, nuts, and dietary spices may reduce the risk of gallstones.
- At least 2‒3 hours of exercise each week can reduce the risk of cholecystectomy by about 20%.
What Natural Interventions May Be Beneficial for Gallstones?
- Vitamin C. Vitamin C decreases oxidative stress, a contributing factor in gallstone formation. Low vitamin C intake has been linked with increased cholesterol concentration in bile, and a study showed regular vitamin C users were 66% less likely to have gallstones than those who did not use it.
- Fish oil and omega-3 fatty acids. Fish oils and omega-3 fatty acids may prevent gallstone formation by preventing crystallization. Supplementation with omega-3 fats was also shown to attenuate the risk of developing gallstones due to rapid weight loss.
- S-adenosylmethionine (SAMe). SAMe has been shown to improve bile flow in people with certain liver diseases. It also may decrease the level of cholesterol in the bile.
- Curcumin. Curcumin, a polyphenolic compound extracted from turmeric, may reduce the chance of gallstones forming by improving cholesterol and lipid metabolism. It can also reduce postoperative pain following a cholecystectomy. However, people with bile duct obstructions should avoid curcumin because it may promote gallbladder contraction.
- Other natural interventions that may help reduce the risk of gallstone formation include iron (in those with iron deficiencies), vitamin E, epigallocatechin gallate (EGCG, a flavonoid found in green tea), melatonin, and milk thistle.
2 Introduction
Gallstones are hard deposits of bile components that form in the gallbladder or bile ducts. Bile is produced by the liver and flows into the gallbladder to be stored until it is needed to help with the digestion and absorption of fat (Maldonado-Valderrama 2011). Signals from the digestive system after eating trigger the release of bile into the small intestine via the bile ducts. Gallstones may cause dull pain and indigestion due to chronic inflammation of the gallbladder, or acute, often severe, pain if they block bile flow. In rare cases, inflammation of the gallbladder, liver, or pancreas resulting from gallstones can become life-threatening (Zakko 2018; Byrne 2006; Indar 2002; Rangaswamy 2017).
Gallstones are very common in Western societies, and their prevalence is increasing. About 38 million people in the United States have gallstones, and one million new diagnoses are made each year (Zakko 2018; Stinton 2012; Ibrahim 2018). However, as many as 80% of gallstone cases are silent, causing no immediate signs or symptoms (Stinton 2012; Jones, Ghassemzadeh 2018; de Bari 2012).
Gallstones can range in size from a tiny speck to as large as a golf ball (Mayo Clinic 2017; Zakko 2018). Most gallstones are composed primarily of cholesterol, but a small percentage are made mainly of bilirubin and are known as pigment stones. Cholesterol gallstones usually form in the gallbladder, but some pigment stones form in the bile ducts (Shaffer 2018).
Gallstones may be associated with increased risks of gallbladder, pancreatic, and colorectal cancers (Pak 2016). In addition, there is mounting evidence that gallstones are a risk factor for cardiovascular disease and increased mortality (Upala 2017; Shabanzadeh, Sorensen, Jorgensen 2017b; Shabanzadeh, Skaaby, Sorensen, Jorgensen 2017; Zheng 2016).
Silent gallstones are often found incidentally and usually left untreated, but surgery is generally recommended in people with symptoms (Jones, Ghassemzadeh 2018). Cholecystectomy (removal of the gallbladder) is one of the most common surgeries in the United States and is done laparoscopically in most cases (Zakko 2018). In some circumstances, treatment with an oral bile salt that gradually softens and dissolves gallstones is the preferred approach (Goral 2016).
In this protocol you will learn how gallstones form and are diagnosed, the available conventional treatment options, and surgical approaches that are continually being refined. You will also learn about diet, lifestyle, and integrative approaches to reducing the risk of gallstones and their complications. For example, eating a diet that emphasizes fiber, fruits and vegetables, plant proteins, and monounsaturated and polyunsaturated fats can help prevent the formation and growth of cholesterol gallstones (Di Ciaula 2017). Physical activity not only protects against gallstones but can also help prevent silent gallstones from becoming problematic (Shabanzadeh, Sorensen, Jorgensen 2017a; Chuang 2001). Gallbladder function may be improved and the risk of cholesterol gallstones further decreased by integrative interventions such as fish oil (Mendez-Sanchez 2001), vitamin C (del Pozo 2014), soy lecithin (Pakula 1996), curcumin from turmeric (Rasyid 2002), and epigallocatechin gallate (EGCG) from green tea (Shan 2008). Finally, emerging evidence suggests medications targeting metabolic disturbances such as high cholesterol and glucose levels may have a role in preventing cholesterol gallstones (Husain 2015; Liao 2017).
3 Background
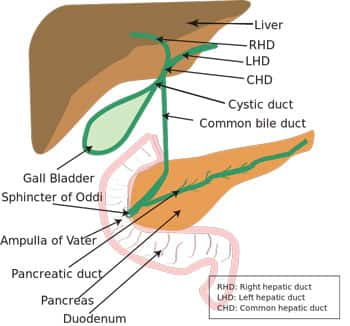
Anatomy of the Biliary System
The gallbladder is a pear-shaped, muscular, pouch-like organ that is roughly three to six inches long and sits under the liver in the upper right region of the abdomen. Some of the bile produced by the liver flows directly into the small intestine, but about 50% flows into the gallbladder where it is stored and concentrated until needed to facilitate fat digestion. Between meals, the gallbladder is relaxed, but during meals, signals from the digestive tract stimulate contractions of the gallbladder and bile is released, through a system of ducts, into the intestine. In addition to helping with digestion, bile carries waste products from the liver to be eliminated through the digestive tract (JHM 2018; Zakko 2018; Housset 2016).
Gallstone Formation
Bile, a greenish-yellow fluid produced in the liver, is made of bile salts, cholesterol, phospholipids (a type of fatty molecule), electrolytes, bilirubin, and water (JHM 2018; Hundt 2018). When excess cholesterol is present in bile, it can crystalize. Sludge forms when cholesterol crystals mix with mucus in the gallbladder. Over time, these crystals can aggregate and form stones (Jones, Ghassemzadeh 2018; Tanaja 2018).
Gallstones that are more than 70% cholesterol are known as cholesterol stones; if cholesterol content is between 30% and 70%, they are called mixed stones; and gallstones with a cholesterol content less than 30% are pigment stones (Molvar 2016). Calcium salts, such as calcium bilirubinate and calcium phosphate, are concentrated in pigment gallstones, making these types of gallstones easy to visualize on an X-ray. Calcium, usually as calcium carbonate, is present in smaller amounts in cholesterol and mixed gallstones (Njeze 2013; Portincasa 2012; Kaufman 1994). As many as 90% of gallstones in people living in Western societies are cholesterol and mixed gallstones that form in the gallbladder (Mayo Clinic 2017; Molvar 2016; Shaffer 2018).
Pigment stones usually form when there is excess bilirubin (ie, yellow pigment produced during the breakdown of red blood cells) in the bile. Conditions such as liver cirrhosis and certain blood disorders can lead to excess bilirubin in the bile and contribute to the formation of black pigment gallstones (Tanaja 2018; Mayo Clinic 2017). Parasitic infections and anatomical narrowing of bile ducts are major causes of brown pigment stones (Shaffer 2018).
Gallbladder Motility and Cholesterol Stone Formation
In the early stages of cholesterol sludge and gallstone formation, the muscular function of the gallbladder weakens, reducing the gallbladder's ability to respond to signals. Lack of bile flow due to low gallbladder motility then further contributes to sludge and stone formation by allowing time for increased cholesterol concentration, crystallization, and aggregation (Tanaja 2018; Jones, Ghassemzadeh 2018; Chen 2015).
Oxidative Stress
Oxidative stress contributes to gallstone development. The process of gallstone formation and growth has been shown to be enhanced in the presence of oxidized bilirubin, which is found in gallstones (Sanikidze 2016; Lichtenberg 1988). People with gallstones often have high levels of oxidized lipids in their blood, and gallbladders removed due to gallstones show high levels of oxidative damage as well as low levels of antioxidant enzymes (Geetha 2002).
Complications of Gallstones
A biliary blockage due to trapped gallstones can lead to acute complications such as (Zakko 2018; Tanaja 2018; Shaffer 2018; Zimmer 2015):
- Cholecystitis: inflammation of the gallbladder
- Choledocholithiasis: one or more gallstones lodged in the common bile duct
- Cholangitis: infection with inflammation in the bile ducts due to an obstruction
- Pancreatitis: inflammation of the pancreas due to obstruction of the pancreatic duct
- Ileus: a rare and dangerous complication wherein the GI tract no longer properly propels ingested food material through the GI tract via peristaltic action. A large gallstone may cause Ileus.
In some cases, gallstones cause chronic inflammation in the gallbladder (chronic cholecystitis), leading to thickening of the gallbladder walls (Jones, Ferguson 2018).
4 Risk Factors
Gallstone formation is influenced by interactions between genetic, metabolic, and environmental factors (Pak 2016). Some of those factors include:
- Diet. A Western-style diet is one of the strongest risk factors for cholesterol gallstones. Specifically, high intakes of calories, carbohydrates, saturated fats, and sugar coupled with low intake of fiber have been linked to increased risk, while consumption of polyunsaturated fats, fiber, fish, fruits and vegetables, and nuts have been associated with lower risk (Pak 2016).
- Age. Risk of developing cholesterol and pigmented stones increases with age (Shaffer 2018; Lee 2015). One reason may be that bile acid production declines with age, leading to greater concentration of cholesterol in bile (Pak 2016). Aging may also be associated with reduced gallbladder motility (Macias 2012).
- Gender. Women have a higher risk of cholesterol gallstones than men. This may be due to the effects of female hormones: estrogens increase cholesterol secretion into bile, and progesterone decreases gallbladder motility. Exposure to elevated levels of female hormones, such as during pregnancy or due to estrogen therapy and possibly oral contraceptives, further increase the risk (Pak 2016; Shaffer 2018; Fogel 2016; Wang, Wang 2017).
- Ethnicity. Native North and South Americans, as well as Mexican Americans, have higher rates of gallstones and gallbladder disease than other ethnic groups. For example, among Native Americans, over 64% of women and nearly 30% of men have gallstones (Stinton 2012). South Asians have a higher risk of brown pigmented gallstones, which are related to bacterial and parasitic infections (Tanaja 2018; Vitek 2012).
- Genetics. Having a family member who has had gallstones is associated with an increased risk, and research suggests some individuals are genetically predisposed to forming cholesterol or pigment gallstones (Shaffer 2018; Lammert 2016).
- Obesity. A higher incidence of cholesterol gallstones is seen in people who are overweight or obese, especially women. The risk is particularly high in those with abdominal obesity (Pak 2016; Sekine 2015).
- Fasting and rapid weight loss. While gradual weight loss may reduce gallstone risk, rapid weight loss increases the risk of gallstone formation. Prolonged fasting and weight cycling (eg, as a result of "yo-yo dieting") are also correlated with higher cholesterol gallstone risk (Pak 2016; Shaffer 2018; Njeze 2013).
- Total parenteral nutrition (TPN). TPN, in which all nutrition is delivered intravenously, is frequently associated with rapid weight loss and lack of gallbladder stimulation, both of which can contribute to gallstone formation (Shaffer 2018).
- Other diseases and conditions. Metabolic syndrome, characterized by a group of cardiovascular risk factors, including insulin resistance, high blood pressure, high blood glucose levels, low HDL cholesterol levels, high triglyceride levels, and abdominal obesity, is associated with increased cholesterol secretion and gallstone formation (Shabanzadeh, Skaaby, Sorensen, Eugen-Olsen 2017; Sang 2016). Celiac disease, which may impair gallbladder function, has also been proposed as a risk factor for cholesterol gallstones (Wang, Liu 2017). Cirrhosis, nonalcoholic fatty liver disease, other liver diseases; cystic fibrosis; and Crohn's disease are also risk factors for gallstones; as are certain blood disorders like sickle cell anemia, beta-thalassemia, and other causes of hemolytic anemia (Shaffer 2018; Stinton 2012; Njeze 2013).
- Medications. Several pharmaceuticals are known to increase the risk of gallstones. In addition to estrogens, these include octreotide (Sandostatin, used mainly to treat acromegaly), ceftriaxone (Rocephin, an antibiotic), and thiazide diuretics (such as hydrochlorothiazide [Apo-hydro], used mainly to treat high blood pressure). On the other hand, statins (such as atorvastatin [Lipitor], used to treat high cholesterol levels) and metformin (Glucophage, used to treat type 2 diabetes) may decrease gallstone risk (Stinton 2012; Liao 2017).
- Sedentary lifestyle. Physical activity protects against cholesterol gallstone formation, possibly by improving gallbladder and gut motility and through positive effects on cholesterol metabolism. It has been suggested that an average of two to three hours of recreational physical activity each week could reduce the chance of needing surgery for gallstone disease by 20% (Pak 2016).
5 Symptoms
Biliary pain is the most common symptom of gallstone disease. Patients typically describe acute, severe pain in the upper-right or upper-mid region of the abdomen, often radiating to the right shoulder or between the shoulder blades. Biliary pain may last for minutes to hours and may occur after eating or be constant (Mayo Clinic 2017; Shaffer 2018; Zakko 2018; Tanaja 2018; Fogel 2016).
Biliary pain that lasts longer than 24 hours points to the possibility of complications of gallstone disease. Certain symptom patterns can help predict the location of the stone and which complication is likely (Fogel 2016):
- Symptoms of acute cholecystitis include nausea, fever, and intense tenderness in the upper-right abdomen (Zakko 2018; Shaffer 2018).
- Symptoms of acute cholangitis, an infection of the bile duct, often include a classic group of signs and symptoms known as Charcot's triad—persistent abdominal pain, fever, and jaundice (Rumsey 2017; Zimmer 2015).
- Symptoms of acute pancreatitis due to gallstone obstruction of the pancreatic duct include pain in the upper-middle abdomen that may radiate to the mid-back. Gallstone pancreatitis may be accompanied by peritonitis (Shaffer 2018), a painful and potentially life-threatening condition in which the lining of the inner abdominal wall becomes inflamed (Mayo Clinic 2015; Banks 2010; Hazem 2009).
Chronic cholecystitis causes tenderness and a dull pain in the upper right abdomen that radiates to the middle of the back. It can also cause digestive symptoms such as gas, bloating, nausea, and occasional vomiting. These symptoms are usually worse after eating fatty foods and often occur in the evening. People with chronic cholecystitis sometimes have acute flare-ups of intense biliary pain (Jones, Ferguson 2018).
6 Diagnosis
Silent gallstones are often found on an abdominal ultrasound that is done for other reasons (Zakko 2018). In symptomatic cases, history-taking and a physical exam are essential to making an accurate diagnosis. Lab tests and imaging are used to confirm the presence of suspected gallstones and help determine whether they are the cause of the presenting symptoms (Zakko 2018; Chen 2012; Wang 2009).
Patients with acute cholecystitis may have fever, jaundice, and strong pain when the upper-right abdomen is pressed while the patient takes a deep breath, which is known as Murphy's sign. These and other signs and symptoms, such as a rapid heart rate and low blood pressure, indicate the possibility of other gallstone-related complications (Shaffer 2018; Tanaja 2018; Indar 2002).
Differential Diagnosis
Several other conditions are important to keep in mind as potential causes of upper-abdominal pain that may resemble symptoms caused by gallstones. These include peptic ulcer disease, non-gallstone-related acute cholecystitis, and non-gallstone-related pancreatitis (Shaffer 2018). Other conditions that can mimic biliary pain include heart attack, aneurysm of the abdominal aorta, gastritis, and hepatitis (Portincasa 2006).
Laboratory Tests
Certain blood tests may help with diagnosis, including (Shaffer 2018; Resnick 2016):
- Complete Blood Count (CBC): The number of white blood cells is often elevated in patients with gallstone complications.
- Alanine Transaminase (ALT) and Alkaline Phosphatase (ALP): Elevated blood levels of these enzymes can be a sign of biliary obstruction. Typically, ALT levels rise quickly and ALP levels rise later.
- Bilirubin: Blood bilirubin level is usually elevated if a bile duct is obstructed.
- Amylase and Lipase: Elevated levels of these pancreatic enzymes suggest pancreatitis.
Imaging
The best initial test for diagnosing gallstones is an abdominal ultrasound (Shaffer 2018; Tanaja 2018). It is highly accurate for detecting stones, can detect sludge as well as stones as small as 2 mm, and identify the presence of acute cholecystitis (Jones, Ghassemzadeh 2018). The ultrasound exam may also detect a dilation of the common bile duct, raising the suspicion of a bile duct stone, obstruction, or tumor (Tanaja 2018; Fogel 2016).
Gallstones with a substantial calcium content may be visible on an X-ray. Computed tomography (CT) and magnetic resonance imaging (MRI) can also detect gallstones, but are less likely than ultrasound to find acute cholecystitis (Jones, Ghassemzadeh 2018). A CT scan may help identify complications such as an abscess or perforation (Shaffer 2018).
A cholescintigraphy scan, also known as a hepatobiliary iminodiacetic acid or HIDA scan, is performed by injecting a radioactive tracer into the blood to evaluate the state of the gallbladder. This scan is used to confirm an unclear diagnosis of acute cholecystitis (Tanaja 2018). A HIDA scan can also be useful for diagnosing chronic cholecystitis and gallbladder motility disorders not related to gallstones (Jones, Ferguson 2018; Goussous 2014).
If ultrasound findings suggest there are gallstones in the common bile duct, an imaging test called magnetic resonance cholangiopancreatography (MRCP) may be used for confirmation (Jones, Ghassemzadeh 2018). An endoscopic ultrasound scan may provide similarly useful information, and is generally used in patients for whom MRCP is not an option, such as those with claustrophobia, as well as certain implanted devices like heart pacemakers or metal joint implants (Shaffer 2018; Pan 2016).
Endoscopic retrograde cholangiopancreatography (ERCP) is another useful diagnostic method. ERCP is an invasive test that involves the use of an injected dye. It can function as both a diagnostic and a therapeutic procedure and is sometimes used in emergency situations involving the bile ducts, since stones can be visualized and removed using this procedure (Shaffer 2018; Tanaja 2018; Lee 2018).
7 Conventional Treatment
Typically, silent gallstones are left untreated, but surgery may be considered for individuals deemed to have a high risk of gallbladder cancer or conditions that increase their risk of gallstone complications, such as sickle cell disease, a weakened immune system, or an upcoming weight loss surgery (Shaffer 2018; Fogel 2016). Dietary, lifestyle, and natural medicine interventions may help people with silent gallstones avoid progressing to a symptomatic stage of gallstone disease (Shabanzadeh 2016; Di Ciaula 2017).
For all forms of symptomatic gallstone disease, surgery is the mainstay of conventional treatment.
Gallbladder Removal (Cholecystectomy)
Acute biliary pain from gallstones, in the absence of complications, can be treated with pain relievers (Tanaja 2018). Because recurrence is common, surgical removal of the gallbladder, known as cholecystectomy, is widely recommended following an acute episode of gallstone cholecystitis (Jones, Ghassemzadeh 2018; Sinha 2002; Acar 2017). Cholecystectomy is also the treatment of choice for chronic cholecystitis (inflammation of the gallbladder) (Jones, Ferguson 2018).
Laparoscopic cholecystectomy, which uses a video camera inserted via small punctures in the abdominal wall, is preferred for its shorter in-hospital time, shorter post-surgical recovery time, and lower rates of certain complications. Nonetheless, open cholecystectomy, involving a larger cut in the abdominal wall, may be necessary in some cases (Shaffer 2018; Zakko 2018; Gomes 2017). About half of individuals who undergo cholecystectomy experience digestive symptoms such as loose stools, gas, and bloating following surgery; these symptoms usually improve over time without treatment (Zakko 2018).
Ursodeoxycholic Acid
The bile salt ursodeoxycholic acid (Actigall), also known as ursodiol, is a naturally-occurring bile salt that decreases liver secretion of cholesterol, lowers cholesterol saturation in bile, and promotes the dissolving of cholesterol stones (Portincasa 2012). Ursodeoxycholic acid usually relieves symptoms within two to three months, but may take years to completely dissolve gallstones (Zakko 2018; Jones, Ghassemzadeh 2018). It is only effective for treating small, cholesterol-rich, calcium-free stones in people with a functioning gallbladder and bile duct. Ursodeoxycholic acid has been reported to have a 90% success rate for dissolving stones with these characteristics; however, the recurrence rate has been reported to be as high as 30–50% within five years after treatment. Because of its slow action and high post-treatment recurrence rate, ursodeoxycholic acid is not widely recommended, and its use is generally reserved for those who cannot undergo surgery (Portincasa 2012; Portincasa 2017; Goral 2016). It is also sometimes prescribed after weight loss surgery to reduce the accompanying risk of gallstone formation (Magouliotis 2017). Mild, temporary diarrhea is the main side effect of ursodeoxycholic acid (Zakko 2018).
Treatment of Gallstone Complications
In patients with gallstones in the common bile duct (choledocholithiasis), stone removal through a combination procedure called endoscopic retrograde cholangiopancreatography (ERCP) with biliary sphincterotomy (cutting of the muscular sphincter that controls bile flow into the small intestine) is considered the best option and is the most commonly used approach. Extra interventions such as stone fragmentation (lithotripsy), balloon dilation of the opening of the common bile duct into the small intestine, or propping open (stenting) the common bile duct may be required along with ERCP if the gallstone is large, impacted, or trapped in front of an obstruction (Molvar 2016; Shaffer 2018; Sakai 2016). Many patients with a stone in a bile duct also have stones in the gallbladder; for these individuals, cholecystectomy is generally performed after ERCP (Shaffer 2018; Baloyiannis 2015).
Bile duct infection (cholangitis) and gallstone pancreatitis are dangerous complications that require immediate attention, including intravenous fluids, pain relievers, and antibiotics. ERCP, stone removal, and sphincterotomy may be needed, and cholecystectomy will likely be recommended during the same hospital stay or at a later time (Shaffer 2018; Stinton 2012). Gallstone-related bowel obstruction (ileus) also requires urgent medical treatment with surgical stone removal and repair of the intestinal wall, and sometimes cholecystectomy either as part of the same procedure or later (Turner 2018).
Health Effects of Cholecystectomy
After cholecystectomy, patients may experience short-term digestive problems, such as diarrhea, bloating, and abdominal pain (Altomare 2017; Zakko 2018). Although pre-surgery symptoms are effectively relieved in more than 90% of patients treated with cholecystectomy, a small number of patients develop a set of symptoms and findings collectively referred to as post-cholecystectomy syndrome (Jaunoo 2010). Dysfunction of the sphincter of Oddi, located at the opening of the common bile duct into the small intestine, is a cause in some cases of post-cholecystectomy syndrome, but more frequently the cause is an overlooked disorder outside of the biliary system, such as peptic ulcer, chronic pancreatitis, or irritable bowel syndrome, or is unknown (Tarnasky 2016; Jaunoo 2010; Shirah 2018). Cholecystectomy is also associated with long-term increased risk of weight gain and metabolic syndrome, gastritis, and deficiencies of fat soluble vitamins (ie, vitamins A, D, E and K) (Altomare 2017; Chen 2018).
8 Novel and Emerging Therapies
Surgery has been the cornerstone of gallstone treatment for many decades (Fogel 2016), but researchers continue to search for new drugs, and new ways to use existing drugs, to prevent gallstones and their complications.
Advances in Non-Surgical Approaches
Medications that affect cholesterol metabolism are currently under investigation for their potential in preventing and treating gallstone disease:
- Ursodeoxycholic acid. As previously noted, ursodeoxycholic acid (or Ursodiol) is currently used to treat gallstone disease in patients for whom surgery is not an option, but widening its use has been proposed, such as to reduce the risk of gallstone formation during pregnancy or rapid weight loss, after abdominal surgery, and in infants requiring long-term total parenteral nutrition (Portincasa 2012; de Bari, Wang, Liu 2014; Stokes 2014; Simic 2014). In addition, synthetic molecules based on ursodeoxycholic acid but with stronger effects have been developed. It is speculated that such bile acid derivatives, and possibly other drugs targeting bile acid activity, may help to better fight gallstone disease (Yu 2016; Halilbasic 2013; Portincasa 2012).
- Metformin. In a study published in 2017, the long-term use of metformin (Glucophage), an anti-diabetic medication, was correlated with a lower risk of gallstones in diabetic subjects (Liao 2017). Metformin's possible gallstone-preventing effects could be related to its ability to improve metabolism. There is also evidence that metformin improves gallbladder motility (Rohde 2016; Isik 2012).
- Statins. Statins are a family of medications used to reduce elevated cholesterol levels. Examples include atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor). Statins work in part by interfering with the synthesis of cholesterol in the liver, and they also reduce the cholesterol saturation of bile (Cariati 2012; Lioudaki 2011). Findings from animal studies suggest statins may be effective for reducing cholesterol gallstone formation. In humans, statin use has been correlated with a lower risk of gallstone disease and cholecystectomy, but results from randomized clinical trials so far have been mixed (Portincasa 2012; Kan 2014).
- Ezetimibe. Ezetimibe (Zetia) is a cholesterol-lowering drug that inhibits cholesterol absorption across the intestinal wall. This leads to reduced cholesterol secretion by the liver, decreased cholesterol saturation in bile, and prevention of crystallization in the gallbladder (de Bari 2012; Portincasa 2017). Ezetimibe has been found to prevent gallstone formation in animal research, including in mice exposed to high estrogen levels, and is therefore under consideration as an option for preventing and treating gallstones in humans (de Bari, Wang, Portincasa 2014; Portincasa 2017).
Because of their complementary actions, a combination drug (Liptruzet) that contains atorvastatin and ezetimibe has also been suggested as a possible treatment for cholesterol gallstones (Husain 2015).
Surgical Advances
Surgical approaches are constantly being refined to reduce invasiveness, improve cosmetic outcomes, reduce post-operative pain and recovery time, and maximize effectiveness. One technique that is gaining acceptance is natural orifice transluminal endoscopic surgery (NOTES) cholecystectomy (Abraham 2014; Nemani 2014). This procedure involves the use of a flexible endoscope which is passed through a natural opening in the body, such as the mouth, anus, or vagina, before crossing into the abdominal cavity (Peng 2016). Most NOTES cholecystectomies are done through the vagina (Abraham 2014). A recent advance in NOTES is the addition of laparoscopic assistance, a so-called hybrid NOTES approach (Bernhardt 2017; Mintz 2007).
NOTES cholecystectomies have demonstrated a high degree of safety and a similar complication rate to standard laparoscopic cholecystectomy. In addition, they may be associated with less post-operative pain and may result in less analgesic use and better cosmetic appearance than other types of cholecystectomy (Borchert 2017; Schwaitzberg 2017; Dhillon 2017; Pohlen 2017).
9 Diet and Lifestyle Interventions
Dietary factors play an important role in the development of cholesterol gallstone disease. In general, a high-calorie, high-fat diet characterized by high intakes of sugar, refined carbohydrates, saturated fat, cholesterol, and trans fats has been linked to an increased risk of gallstones and their complications (Compagnucci 2016; Di Ciaula 2017; Di Ciaula 2013; Setiawan 2017). On the other hand, a diet rich in fiber, fruits and vegetables, plant proteins, and monounsaturated and polyunsaturated fats is protective (Di Ciaula 2017; Gaby 2009; Sachdeva 2011). A Mediterranean-style diet, which emphasizes fruits, vegetables, seafood, legumes, and olive oil, was associated with reduced cholecystectomy risk in a study in French women (Barre 2017). A high-fiber diet has been found to prevent gallstones in obese patients undergoing rapid weight loss (Sulaberidze 2014). Some evidence suggests that some of these dietary factors do not appear to impact gallstone risk in pregnant women (Mathew 2015; Basso 1992).
Judicious Weight Loss
Weight loss is an important strategy for reducing the risk of gallstones in overweight or obese individuals, yet the risk of gallstones increases when weight is lost rapidly (Portincasa 2016). In a study with more than 6,000 people participating in one of two weight loss programs, those on a 500 calorie per day diet for three months, followed by nine months of weight maintenance, were three times more likely to need hospitalization for symptomatic gallstones or cholecystectomy for gallstones than those who started with a 1,200–1,500 calorie per day diet. Although the rates of gallstone-related hospitalization were relatively low in both groups, at 1.5% per year in those on the very-low-calorie diet and 0.4% per year in those on the low-calorie diet, the results suggest that the health benefits of weight loss may be best achieved through modest calorie restriction (Johansson 2014).
Generally, weight loss of greater than 24% of initial body weight and at a rate greater than 1.5 kg (about 3.3 pounds) per week has been identified as a risk factor for gallstones, but the risk may be mitigated by controlling the rate of weight loss, reducing the length of the overnight fast, and keeping a small amount of fat (at least 7 grams per day) in the diet to improve gallbladder motility (Erlinger 2000).
Specific Foods
Coffee and tea appear to reduce the risk of gallstones, possibly by stimulating gallbladder activity (Zhang 2006; Zhang 2015). Moderate alcohol intake, which may stimulate gallbladder emptying, has also been associated with a lower gallstone risk (Mostofsky 2016; Walcher 2010). Foods that contain polyunsaturated fats (eg, fish) and monounsaturated fats (eg, olive oil and nuts) appear to be protective as well (Misciagna 1996; Brown 2017; Alarcon de la Lastra 2001). In a study that followed over 80,000 women for 20 years, eating five or more servings of nuts per week was associated with a 25% lower risk of cholecystectomy (Tsai 2004a). Similarly, a study that followed over 43,000 men for more than 10 years identified a 30% lower gallstone risk in those eating five or more servings of nuts per week compared with those who rarely or never ate nuts (Ros 2010; Tsai 2004b).
Garlic, onions, fenugreek, and components from other dietary spices including turmeric, cayenne, and black pepper have each demonstrated the ability to prevent and dissolve cholesterol gallstones in animal studies. Preclinical research suggests they reduce cholesterol saturation in bile and inhibit the first stage of cholesterol crystal formation (Song 2015; Shubha 2011; Reddy 2011a; Reddy 2011b; Vidyashankar 2010a; Vidyashankar 2010b).
Physical Activity
A sedentary lifestyle increases the risk of cholesterol gallstones, while being physically active decreases the risk (Stinton 2012). Physical activity may prevent cholesterol gallstone formation by improving gut motility and through positive effects on cholesterol metabolism (Pak 2016). A systematic review and meta-analysis that included eight studies and a combined total of almost 7,000 participants concluded that those with the highest physical activity level had a 25% lower risk of gallbladder disease, including gallstones and cholecystitis, than those with the lowest physical activity level (Aune 2016). Exercise may prevent silent gallstones (Henao-Moran 2014) as well as gallstone complications (Shabanzadeh, Sorensen, Jorgensen 2017a). Two to three hours of recreational physical activity each week may reduce the risk of cholecystectomy by about 20% (Pak 2016).
10 Nutrients
Nutritional supplements hold much promise in preventing cholesterol gallstones and their complications. Individuals with a high gallstone risk due to ethnicity, gender, age, family history, or other health and medical factors, and those with known silent gallstones, may want to consider supplements to possibly reduce their risk.
Primary Suggestions
Vitamin C
Vitamin C is a water-soluble vitamin that is well known for neutralizing free radicals and decreasing oxidative stress, a contributing factor in gallstone formation (Sanikidze 2016; del Pozo 2014). Vitamin C is also needed for the conversion of cholesterol into bile acids (Gaby 2009). The ability of vitamin C to prevent gallstone formation is supported by several animal studies. A relationship between vitamin C deficiency and gallstones has been recognized since the 1970s (Ginter 1971) and, for decades, low intake has been implicated in raising cholesterol saturation in the bile and in increasing the likelihood of gallstone formation (Simon 1993; Worthington 1997; Ginter 1973).
In a controlled clinical trial, 16 gallstone patients scheduled for cholecystectomy were given 500 mg of supplemental vitamin C four times daily for two weeks before surgery. Compared with similar patients who did not supplement with vitamin C, the study subjects had improved bile composition and a lengthening of the time required for cholesterol crystals to form (Gustafsson 1997). Another trial found a similar effect in 13 patients awaiting cholecystectomy who were taking 1 gram of vitamin C twice daily (del Pozo 2014). In an observational study of 2,129 subjects, regular vitamin C users were 66% less likely to have gallstones than non-vitamin C users when assessed by abdominal ultrasound (Walcher 2009). The correlation between vitamin C levels and gallstone risk appears to be stronger in women than in men (Simon 2000; Simon 1998; Ortega 1997).
Fish Oil and Omega-3 Fatty Acids
Supplementing with fish oil or omega-3 polyunsaturated fatty acids from fish (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) may prevent gallstones by improving bile composition and preventing crystal formation (Berr 1992; Jonkers 2006; Cho 2015; Pasternak 2017). In a double-blind placebo-controlled trial, 35 obese women with no history of gallstones or cholecystectomy were treated with a 1,200 calorie per day diet, along with either 11.3 grams per day of omega-3 fats from fish, ursodeoxycholic acid, or placebo for six weeks. While on the diet, the time needed for cholesterol crystals to form decreased in the placebo and ursodeoxycholic acid groups, but not in the omega-3 group, suggesting fish oil may prevent the increase in gallstone risk seen with low-calorie weight loss dieting (Mendez-Sanchez 2001).
S-Adenosylmethionine (SAMe)
S-adenosylmethionine (SAMe) exerts protective effects on the liver and improves bile flow in people with certain liver diseases (Almasio 1990). In a preliminary study that included seven women with a history of biliary problems during pregnancy, taking 800 mg oral SAMe daily for two weeks resulted in decreased cholesterol saturation in the bile (Frezza 1988). In a trial in six healthy women who had experienced an increase in bile cholesterol saturation after starting oral contraceptives, the addition of 600 mg SAMe daily for two cycles of contraceptive use reduced this effect (Di Padova 1984).
Curcumin
Curcumin is a carotenoid extracted from turmeric. Several animal studies suggest curcumin may reduce the likelihood of gallstone formation by improving cholesterol and lipid metabolism (Srinivasan 2017). Curcumin has also been shown to enhance gallbladder motility (Rasyid 2002; Rasyid 1999), reduce gallbladder inflammation, and normalize bile acid metabolism (Yang 2016). In mice fed a high-fat high-cholesterol diet, curcumin protected against the development of gallstones, and its effect was enhanced with the addition of piperine, an alkaloid from black pepper (Li 2015).
Curcumin may also be helpful in recovery after cholecystectomy. In a randomized controlled trial, 50 patients undergoing laparoscopic cholecystectomy were given either curcumin or a placebo, along with standard pain relievers to use as needed, upon hospital discharge. The curcumin group had less post-operative pain and fatigue and used less pain-relieving medication than the placebo group (Agarwal 2011).
Curcumin has been shown in a few studies to promote gallbladder contraction (Rasyid 1999; Rasyid 2002). Therefore, people with a history of bile duct obstruction or who have an active obstruction should avoid curcumin.
Additional Suggestions
Iron
Individuals with iron-deficiency anemia have been found to have a higher risk of gallstones than those with normal iron levels (Pamuk 2009). This relationship has been verified in the reverse as well: gallstone patients have been found to be more likely to have low serum iron levels than healthy individuals (Prasad 2015). On the other hand, concentrations of iron in the blood and bile have been reported to be significantly higher in people with pigment gallstones (Khan 2017), which are often related to conditions marked by increased red blood cell breakdown (Stinton 2012).
Iron deficiency may alter the activities of several liver enzymes, leading to increased cholesterol saturation in bile and increased cholesterol crystallization, and it also negatively impacts gallbladder motility (Prasad 2015). In addition, it is possible that gallstone disease contributes to iron malabsorption and poor iron status (Saboor 2015).
Different forms of dietary iron may have varying impacts on gallstone formation. One study followed over 44,000 men for 16 years and examined their iron consumption using a food questionnaire. Participants with the highest intake of heme iron, a well-absorbed, protein-bound form of iron found in meat and seafood, had a 21% higher risk of symptomatic gallstones compared with those with the lowest intake, but there was no significant link between the intake of non-heme iron, which is found predominantly in plant-based foods, and symptomatic gallstones (Tsai 2007). Dietary heme iron has also been shown to increase the burden of oxidative stress in the body (Romeu 2013).
Because of the role of excess iron in raising oxidative stress and the risk of cardiovascular disease, it is important to have one’s iron status assessed before taking an iron supplement (Kraml 2017). Only those with iron deficiency should consider iron supplementation to reduce the risk of gallstones.
Vitamin E
Vitamin E is a fat-soluble nutrient that helps prevent and repair oxidative damage to lipids in the body. Vitamin E is a term that collectively refers to four tocopherols (alpha, beta, gamma, and delta) and four tocotrienols (alpha, beta, gamma, and delta), with alpha-tocopherol being the predominant form in the body (Jiang 2001; Jiang 2014). Observational studies have noted that individuals with gallstones have lower blood levels of alpha-tocopherol and alpha-tocopherol/cholesterol ratios, and lower dietary intake of alpha-tocopherol, as compared with unaffected individuals (Waniek 2018; Worthington 1997; Worthington 2004). Since oxidative stress is one of the factors believed to contribute to a higher risk of gallstones, supplementing with vitamin E may be beneficial for preventing gallstones (Waniek 2018; Sanikidze 2016).
Epigallocatechin Gallate (EGCG)
Epigallocatechin gallate, or EGCG, is a green tea flavonoid. EGCG has demonstrated gallstone-preventing effects in a mouse model of gallstone disease, possibly through its anti-inflammatory activity (Shan 2008). Findings from a population-based case-control study in China suggest drinking tea may reduce the risks of gallstone disease and gallbladder cancer (Zhang 2006). However, other research has not found a clear connection between tea drinking and gallstones (Ishizuk 2003).
Melatonin
Melatonin, a neuro-hormone produced in the pineal gland, may have a role in gallstone disease prevention or treatment due to its anti-inflammatory and free-radical-scavenging properties, as well as its beneficial effect on gallbladder muscle tone (Pozo 2010; Koppisetti 2008). In animal and laboratory research, melatonin has been shown to reverse age-related muscle dysfunction of the gallbladder and improve inflammation and gallbladder function in acute cholecystitis (Gomez-Pinilla 2006; Gomez-Pinilla 2007; Gomez-Pinilla 2008). In a guinea pig model, the administration of melatonin prevented the formation of pigment gallstones (Shiesh 2000).
Milk Thistle
Silymarin, a flavonoid extract from milk thistle (Silybum marianum), has been shown to counteract the negative impact of estrogen on bile flow in rats (Crocenzi 2001). Silymarin and silybin, its major active component, have also been noted to reduce bile cholesterol content in both rats and human subjects (Nassuato 1983; Nassuato 1991), suggesting its potential value in gallstone prevention and treatment.
Disclaimer and Safety Information
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional. Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website. The protocols described on this website are for adults only, unless otherwise specified. Product labels may contain important safety information and the most recent product information provided by the product manufacturers should be carefully reviewed prior to use to verify the dose, administration, and contraindications. National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from this protocol and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. Life Extension has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in the literature.
References
Abraham S, Rivero HG, Erlikh IV, Griffith LF, Kondamudi VK. Surgical and nonsurgical management of gallstones. American family physician. May 15 2014;89(10):795-802.
Acar T, Kamer E, Acar N, Atahan K, Bag H, Haciyanli M, Akgul O. Laparoscopic cholecystectomy in the treatment of acute cholecystitis: comparison of results between early and late cholecystectomy. The Pan African medical journal. 2017;26:49.
Agarwal KA, Tripathi CD, Agarwal BB, Saluja S. Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surgical endoscopy. Dec 2011;25(12):3805-3810.
Alarcon de la Lastra C, Barranco MD, Motilva V, Herrerias JM. Mediterranean diet and health: biological importance of olive oil. Current pharmaceutical design. Jul 2001;7(10):933-950.
Almasio P, Bortolini M, Pagliaro L, Coltorti M. Role of S-adenosyl-L-methionine in the treatment of intrahepatic cholestasis. Drugs. 1990;40 Suppl 3:111-123.
Altomare DF, Rotelli MT, Palasciano N. Diet after cholecystectomy. Current medicinal chemistry. May 17 2017.
Aune D, Leitzmann M, Vatten LJ. Physical Activity and the Risk of Gallbladder Disease: A Systematic Review and Meta-Analysis of Cohort Studies. Journal of physical activity & health. Jul 2016;13(7):788-795.
Baloyiannis I, Tzovaras G. Current status of laparoendoscopic rendezvous in the treatment of cholelithiasis with concomitant choledocholithiasis. World Journal of Gastrointestinal Endoscopy. Jun 25 2015;7(7):714-719.
Banks PA, Conwell DL, Toskes PP. The management of acute and chronic pancreatitis. Gastroenterology & hepatology. Feb 2010;6(2 Suppl 3):1-16.
Barre A, Gusto G, Cadeau C, Carbonnel F, Boutron-Ruault MC. Diet and Risk of Cholecystectomy: A Prospective Study Based on the French E3N Cohort. The American journal of gastroenterology. Sep 2017;112(9):1448-1456.
Basso L, McCollum PT, Darling MR, Tocchi A, Tanner WA. A descriptive study of pregnant women with gallstones. Relation to dietary and social habits, education, physical activity, height, and weight. European journal of epidemiology. Sep 1992;8(5):629-633.
Behar J, Corazziari E, Guelrud M, Hogan W, Sherman S, Toouli J. Functional gallbladder and sphincter of oddi disorders. Gastroenterology. Apr 2006;130(5):1498-1509.
Bernhardt J, Sasse S, Ludwig K, Meier PN. Update in Natural Orifice Translumenal Endoscopic Surgery (NOTES). Current opinion in gastroenterology. Sep 2017;33(5):346-351.
Berr F, Holl J, Jungst D, Fischer S, Richter WO, Seifferth B, Paumgartner G. Dietary N-3 polyunsaturated fatty acids decrease biliary cholesterol saturation in gallstone disease. Hepatology. Oct 1992;16(4):960-967.
Borchert DH, Federlein M, Ruckbeil O, Schope J. Less pain after transvaginal cholecystectomy: single-center pooled analysis. Surgical endoscopy. Jun 2017;31(6):2573-2576.
Breneman JC. Allergy elimination diet as the most effective gallbladder diet. Annals of allergy. Feb 1968;26(2):83-87.
Brown RC, Gray AR, Tey SL, Chisholm A, Burley V, Greenwood DC, Cade J. Associations between Nut Consumption and Health Vary between Omnivores, Vegetarians, and Vegans. Nutrients. Nov 6 2017;9(11).
Byrne MF. Gallstone pancreatitis--who really needs an ERCP? Canadian journal of gastroenterology = Journal canadien de gastroenterologie. Jan 2006;20(1):15-17.
Cafasso DE, Smith RR. Symptomatic cholelithiasis and functional disorders of the biliary tract. The Surgical clinics of North America. Apr 2014;94(2):233-256.
Cariati A, Piromalli E. Limits and perspective of oral therapy with statins and aspirin for the prevention of symptomatic cholesterol gallstone disease. Expert opinion on pharmacotherapy. Jun 2012;13(9):1223-1227.
Chen LY, Qiao QH, Zhang SC, Chen YH, Chao GQ, Fang LZ. Metabolic syndrome and gallstone disease. World journal of gastroenterology. Aug 21 2012;18(31):4215-4220.
Chen Y, Kong J, Wu S. Cholesterol gallstone disease: focusing on the role of gallbladder. Laboratory investigation; a journal of technical methods and pathology. Feb 2015;95(2):124-131.
Chen Y, Wu S, Tian Y. Cholecystectomy as a risk factor of metabolic syndrome: from epidemiologic clues to biochemical mechanisms. Laboratory investigation; a journal of technical methods and pathology. Jan 2018;98(1):7-14.
Cho SM, Park JA, Kim NH, Kim DS, Zhang D, Yi H, . . . Shin HC. Effect of eicosapentaenoic acid on cholesterol gallstone formation in C57BL/6J mice. Molecular medicine reports. Jan 2015;11(1):362-366.
Chuang CZ, Martin LF, LeGardeur BY, Lopez A. Physical activity, biliary lipids, and gallstones in obese subjects. The American journal of gastroenterology. Jun 2001;96(6):1860-1865.
Compagnucci AB, Perroud HA, Batalles SM, Villavicencio R, Brasca A, Berli D, Pezzotto SM. A nested case-control study on dietary fat consumption and the risk for gallstone disease. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association. Jun 2016;29(3):338-344.
Crocenzi FA, Sanchez Pozzi EJ, Pellegrino JM, Favre CO, Rodriguez Garay EA, Mottino AD, . . . Roma MG. Beneficial effects of silymarin on estrogen-induced cholestasis in the rat: a study in vivo and in isolated hepatocyte couplets. Hepatology. Aug 2001;34(2):329-339.
de Bari O, Neuschwander-Tetri BA, Liu M, Portincasa P, Wang DQ. Ezetimibe: its novel effects on the prevention and the treatment of cholesterol gallstones and nonalcoholic Fatty liver disease. Journal of lipids. 2012;2012:302847.
de Bari O, Wang HH, Portincasa P, Paik CN, Liu M, Wang DQ. Ezetimibe prevents the formation of oestrogen-induced cholesterol gallstones in mice. European journal of clinical investigation. Dec 2014;44(12):1159-1168.
de Bari O, Wang TY, Liu M, Paik CN, Portincasa P, Wang DQ. Cholesterol cholelithiasis in pregnant women: pathogenesis, prevention and treatment. Annals of hepatology. Nov-Dec 2014;13(6):728-745.
del Pozo R, Munoz M, Dumas A, Tapia C, Munoz K, Fuentes F, . . . Jungst D. [Effects of vitamin C administration on cholesterol gallstone formation]. Revista medica de Chile. Jan 2014;142(1):20-26.
Dhillon KS, Awasthi D, Dhillon AS. Natural orifice transluminal endoscopic surgery (hybrid) cholecystectomy: The Dhillon technique. Journal of minimal access surgery. Jul-Sep 2017;13(3):176-181.
Dhiman RK, Chawla YK. Is there a link between oestrogen therapy and gallbladder disease? Expert opinion on drug safety. Jan 2006;5(1):117-129.
Di Ciaula A, Garruti G, Fruhbeck G, De Angelis M, De Bari O, D QHW, . . . Portincasa P. The Role Of Diet In The Pathogenesis Of Cholesterol Gallstones. Current medicinal chemistry. May 29 2017.
Di Ciaula A, Wang DQ, Bonfrate L, Portincasa P. Current views on genetics and epigenetics of cholesterol gallstone disease. Cholesterol. 2013;2013:298421.
Di Padova C, Tritapepe R, Di Padova F, Frezza M, Stramentinoli G. S-adenosyl-L-methionine antagonizes oral contraceptive-induced bile cholesterol supersaturation in healthy women: preliminary report of a controlled randomized trial. The American journal of gastroenterology. Dec 1984;79(12):941-944.
Erlinger S. Gallstones in obesity and weight loss. European journal of gastroenterology & hepatology. Dec 2000;12(12):1347-1352.
Fogel ELS, S. Diseases od the Gallbladder and Bile Ducts. In: Goldman L, Schafer A, eds. Goldman-Cecil Medicine. 25th edition. Philadelphia: Pennsylvania: Elsevier/Saunders; 2016:1038–1048. 2016.
Francis G, Baillie J. Gallbladder dyskinesia: fact or fiction? Current gastroenterology reports. Apr 2011;13(2):188-192.
Fraquelli M, Pagliarulo M, Colucci A, Paggi S, Conte D. Gallbladder motility in obesity, diabetes mellitus and coeliac disease. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. Jul 2003;35 Suppl 3:S12-16.
Frezza M, Tritapepe R, Pozzato G, Di Padova C. Prevention of S-adenosylmethionine of estrogen-induced hepatobiliary toxicity in susceptible women. The American journal of gastroenterology. Oct 1988;83(10):1098-1102.
Gaby AR. Nutritional approaches to prevention and treatment of gallstones. Alternative medicine review: a journal of clinical therapeutic. Sep 2009;14(3):258-267.
Geetha A. Evidence for oxidative stress in the gall bladder mucosa of gall stone patients. Journal of biochemistry, molecular biology, and biophysics : JBMBB : the official journal of the Federation of Asian and Oceanian Biochemists and Molecular Biologists (FAOBMB). Dec 2002;6(6):427-432.
George J, Baillie J. Biliary and gallbladder dyskinesia. Current treatment options in gastroenterology. Aug 2007;10(4):322-327.
Ginter E. Cholesterol: vitamin C controls its transformation to bile acids. Science (New York, N.Y.). Feb 16 1973;179(4074):702-704.
Ginter E. Vitamin-C deficiency and gallstone formation. Lancet (London, England). Nov 27 1971;2(7735):1198-1199.
Gomes CA, Junior CS, Di Saverio S, Sartelli M, Kelly MD, Gomes CC, . . . Guimaraes SF. Acute calculous cholecystitis: Review of current best practices. World journal of gastrointestinal surgery. May 27 2017;9(5):118-126.
Gomez-Pinilla PJ, Camello PJ, Pozo MJ. Effects of melatonin on gallbladder neuromuscular function in acute cholecystitis. The Journal of pharmacology and experimental therapeutics. Oct 2007;323(1):138-146.
Gomez-Pinilla PJ, Camello PJ, Pozo MJ. Protective effect of melatonin on Ca2+ homeostasis and contractility in acute cholecystitis. Journal of pineal research. Apr 2008;44(3):250-260.
Gomez-Pinilla PJ, Camello-Almaraz C, Moreno R, Camello PJ, Pozo MJ. Melatonin treatment reverts age-related changes in Guinea pig gallbladder neuromuscular transmission and contractility. The Journal of pharmacology and experimental therapeutics. Nov 2006;319(2):847-856.
Goral V. Gallstone Etiopathogenesis, Lith and Mucin Genes and New Treatment Approaches. Asian Pacific journal of cancer prevention: APJCP. 2016;17(2):467-471.
Goussous N, Kowdley GC, Sardana N, Spiegler E, Cunningham SC. Gallbladder dysfunction: how much longer will it be controversial? Digestion. 2014;90(3):147-154.
Gustafsson U, Wang FH, Axelson M, Kallner A, Sahlin S, Einarsson K. The effect of vitamin C in high doses on plasma and biliary lipid composition in patients with cholesterol gallstones: prolongation of the nucleation time. European journal of clinical investigation. May 1997;27(5):387-391.
Halilbasic E, Claudel T, Trauner M. Bile acid transporters and regulatory nuclear receptors in the liver and beyond. Journal of hepatology. Jan 2013;58(1):155-168.
Hazem ZM. Acute biliary pancreatitis: diagnosis and treatment. Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association. Jul-Sep 2009;15(3):147-155.
Henao-Moran S, Denova-Gutierrez E, Moran S, Duque X, Gallegos-Carrillo K, Macias N, Salmeron J. Recreational physical activity is inversely associated with asymptomatic gallstones in adult Mexican women. Annals of hepatology. Nov-Dec 2014;13(6):810-818.
Housset C, Chretien Y, Debray D, Chignard N. Functions of the Gallbladder. Comprehensive Physiology. Jun 13 2016;6(3):1549-1577.
Hundt M, John S. Physiology, Bile Secretion. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
Husain NE, Hassan AT, Elmadhoun WM, Ahmed MH. Evaluating the safety of Liptruzet (ezetimibe and atorvastatin): what are the potential benefits beyond low-density lipoprotein cholesterol-lowering effect? Expert opinion on drug safety. 2015;14(9):1445-1455.
Ibrahim M, Sarvepalli S, Morris-Stiff G, Rizk M, Bhatt A, Walsh RM, . . . Burke CA. Gallstones: Watch and wait, or intervene? Cleveland Clinic journal of medicine. Apr 2018;85(4):323-331.
Indar AA, Beckingham IJ. Acute cholecystitis. BMJ (Clinical research ed.). Sep 21 2002;325(7365):639-643.
Ishizuk H, Eguchi H, Oda T, Ogawa S, Nakagawa K, Honjo S, Kono S. Relation of coffee, green tea, and caffeine intake to gallstone disease in middle-aged Japanese men. European journal of epidemiology. 2003;18(5):401-405.
Isik S, Ozcan HN, Ozuguz U, Berker D, Tutuncu Y, Akbaba G, Guler S. Impaired gallbladder motility and the effect of metformin therapy in patients with polycystic ovary syndrome. Clinical endocrinology. Mar 2012;76(3):373-378.
Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). International journal of surgery (London, England). 2010;8(1):15-17.
JHM. Johns Hopkins Medicine. Health Library: Biliary System: Anatomy and Functions. Available at www.hopkinsmedicine.org. Accessed 03/13/18. 2018.
Jiang Q. Natural forms of vitamin E: metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy. Free radical biology & medicine. Jul 2014;72:76-90.
Jiang Q, Christen S, Shigenaga MK, Ames BN. gamma-tocopherol, the major form of vitamin E in the US diet, deserves more attention. The American journal of clinical nutrition. Dec 2001;74(6):714-722.
Johansson K, Sundstrom J, Marcus C, Hemmingsson E, Neovius M. Risk of symptomatic gallstones and cholecystectomy after a very-low-calorie diet or low-calorie diet in a commercial weight loss program: 1-year matched cohort study. International journal of obesity (2005). Feb 2014;38(2):279-284.
Jones MW, Ferguson T. Gallbladder, Cholecystitis, Chronic. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
Jones MW, Ghassemzadeh S. Gallbladder, Gallstones (Calculi). StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
Jonkers IJ, Smelt AH, Princen HM, Kuipers F, Romijn JA, Boverhof R, . . . Stellaard F. Fish oil increases bile acid synthesis in male patients with hypertriglyceridemia. The Journal of nutrition. Apr 2006;136(4):987-991.
Kan HP, Guo WB, Tan YF, Zhou J, Liu CD, Huang YQ. Statin use and risk of gallstone disease: A meta-analysis. Hepatology research : the official journal of the Japan Society of Hepatology. Oct 9 2014.
Kaufman HS, Magnuson TH, Pitt HA, Frasca P, Lillemoe KD. The distribution of calcium salt precipitates in the core, periphery and shell of cholesterol, black pigment and brown pigment gallstones. Hepatology. May 1994;19(5):1124-1132.
Khan M, Kazi TG, Afridi HI, Sirajuddin, Bilal M, Akhtar A, . . . Kadar S. Variation of calcium, copper and iron levels in serum, bile and stone samples of patients having different types of gallstone: A comparative study. Clinica chimica acta; international journal of clinical chemistry. Aug 2017;471:254-262.
Koppisetti S, Jenigiri B, Terron MP, Tengattini S, Tamura H, Flores LJ, . . . Reiter RJ. Reactive oxygen species and the hypomotility of the gall bladder as targets for the treatment of gallstones with melatonin: a review. Digestive diseases and sciences. Oct 2008;53(10):2592-2603.
Kraml P. The role of iron in the pathogenesis of atherosclerosis. Physiological research. Apr 5 2017;66(Supplementum 1):S55-s67.
Lammert F, Gurusamy K, Ko CW, Miquel JF, Mendez-Sanchez N, Portincasa P, . . . Wang DQ. Gallstones. Nature reviews. Disease primers. Apr 28 2016;2:16024.
Lee HS, Chung MJ, Park JY, Bang S, Park SW, Song SY, Chung JB. Urgent endoscopic retrograde cholangiopancreatography is not superior to early ERCP in acute biliary pancreatitis with biliary obstruction without cholangitis. PloS one. 2018;13(2):e0190835.
Lee JY, Keane MG, Pereira S. Diagnosis and treatment of gallstone disease. The Practitioner. Jun 2015;259(1783):15-19, 12.
Li Y, Li M, Wu S, Tian Y. Combination of curcumin and piperine prevents formation of gallstones in C57BL6 mice fed on lithogenic diet: whether NPC1L1/SREBP2 participates in this process? Lipids in health and disease. Sep 3 2015;14:100.
Liao KF, Chuang HY, Lai SW. Metformin Use Correlates with Reduced Risk of Gallstones in Diabetic Patients: A 12-Year Follow-up Study. Frontiers in pharmacology. 2017;8:765.
Lichtenberg D, Ragimova S, Peled Y, Halpern Z. Phospholipid peroxidation as a factor in gallstone pathogenesis. FEBS letters. Feb 8 1988;228(1):179-181.
Lioudaki E, Ganotakis ES, Mikhailidis DP. Lipid lowering drugs and gallstones: a therapeutic option? Current pharmaceutical design. Nov 2011;17(33):3622-3631.
Macias B, Gomez-Pinilla PJ, Camello-Almaraz C, Pascua P, Tresguerres JA, Camello PJ, Pozo MJ. Aging impairs Ca(2+) sensitization pathways in gallbladder smooth muscle. Age. Aug 2012;34(4):881-893.
Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Chatedaki C, Sioka E, Zacharoulis D. Ursodeoxycholic Acid in the Prevention of Gallstone Formation After Bariatric Surgery: an Updated Systematic Review and Meta-analysis. Obesity surgery. Nov 2017;27(11):3021-3030.
Maldonado-Valderrama J, Wilde P, Macierzanka A, Mackie A. The role of bile salts in digestion. Advances in colloid and interface science. Jun 9 2011;165(1):36-46.
Mathew LK, Ko C. Dietary fat and protein intake are not associated with incident biliary sludge and stones during pregnancy. JPEN. Journal of parenteral and enteral nutrition. Jan 2015;39(1):124-128.
Mayo Clinic. Diseases and Conditions: Gallstones. Available at https://www.mayoclinic.org/diseases-conditions/gallstones/symptoms-causes/syc-20354214?p=1 and https://www.mayoclinic.org/diseases-conditions/gallstones/diagnosis-treatment/drc-20354220?p=1. Published 11/17/2017. Accessed 03/13/2018.
Mayo Clinic. Diseases and Conditions: Peritonitis. Available at https://www.mayoclinic.org/diseases-conditions/peritonitis/symptoms-causes/syc-20376247?p=1. Published 03/31/2015. Accessed 03/13/2018. 2015.
Mendez-Sanchez N, Gonzalez V, Aguayo P, Sanchez JM, Tanimoto MA, Elizondo J, Uribe M. Fish oil (n-3) polyunsaturated fatty acids beneficially affect biliary cholesterol nucleation time in obese women losing weight. The Journal of nutrition. Sep 2001;131(9):2300-2303.
Mintz Y, Horgan S, Cullen J, Ramamoorthy S, Chock A, Savu MK, . . . Talamini MA. NOTES: the hybrid technique. Journal of laparoendoscopic & advanced surgical techniques. Part A. Aug 2007;17(4):402-406.
Misciagna G, Leoci C, Guerra V, Chiloiro M, Elba S, Petruzzi J, . . . Giorgio I. Epidemiology of cholelithiasis in southern Italy. Part II: Risk factors. European journal of gastroenterology & hepatology. Jun 1996;8(6):585-593.
Molvar C, Glaenzer B. Choledocholithiasis: Evaluation, Treatment, and Outcomes. Seminars in interventional radiology. Dec 2016;33(4):268-276.
Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB. Key Findings on Alcohol Consumption and a Variety of Health Outcomes From the Nurses' Health Study. American journal of public health. Sep 2016;106(9):1586-1591.
Nassuato G, Iemmolo RM, Lirussi F, Orlando R, Giacon L, Venuti M, . . . Okolicsanyi L. Effect of Silybin on biliary lipid composition in rats. Pharmacological research communications. Apr 1983;15(4):337-346.
Nassuato G, Iemmolo RM, Strazzabosco M, Lirussi F, Deana R, Francesconi MA, . . . et al. Effect of Silibinin on biliary lipid composition. Experimental and clinical study. Journal of hepatology. May 1991;12(3):290-295.
Nemani A, Sankaranarayanan G, Olasky JS, Adra S, Roberts KE, Panait L, . . . De S. A comparison of NOTES transvaginal and laparoscopic cholecystectomy procedures based upon task analysis. Surgical endoscopy. Aug 2014;28(8):2443-2451.
Njeze GE. Gallstones. Nigerian Journal of Surgery : Official Publication of the Nigerian Surgical Research Society. Jul-Dec 2013;19(2):49-55.
Ortega RM, Fernandez-Azuela M, Encinas-Sotillos A, Andres P, Lopez-Sobaler AM. Differences in diet and food habits between patients with gallstones and controls. Journal of the American College of Nutrition. Feb 1997;16(1):88-95.
Pak M, Lindseth G. Risk Factors for Cholelithiasis. Gastroenterology nursing : the official journal of the Society of Gastroenterology Nurses and Associates. Jul-Aug 2016;39(4):297-309.
Pakula R, Konikoff FM, Rubin M, Ringel Y, Peled Y, Tietz A, Gilat T. The effects of dietary phospholipids enriched with phosphatidylethanolamine on bile and red cell membrane lipids in humans. Lipids. March 01 1996;31(3):295-303.
Pamuk GE, Umit H, Harmandar F, Yesil N. Patients with iron deficiency anemia have an increased prevalence of gallstones. Annals of hematology. Jan 2009;88(1):17-20.
Pan S, Guo Q. Endoscopic ultrasonography versus magnetic resonance cholangiopancreatography for suspected choledocholithiasis: Comments from the radiologists'. Endoscopic ultrasound. Mar-Apr 2016;5(2):129-131.
Pasternak A, Bugajska J, Szura M, Walocha JA, Matyja A, Gajda M, . . . Gil K. Biliary Polyunsaturated Fatty Acids and Telocytes in Gallstone Disease. Cell transplantation. Jan 24 2017;26(1):125-133.
Peng C, Ling Y, Ma C, Ma X, Fan W, Niu W, Niu J. Safety Outcomes of NOTES Cholecystectomy Versus Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Surgical laparoscopy, endoscopy & percutaneous techniques. Oct 2016;26(5):347-353.
Pohlen U, Feller A, Holmer C. Transvaginal Hybrid NOTES Cholecystectomy: A Single-Centre Long-Term Experience on Sexual Function. World journal of surgery. Dec 21 2017.
Portincasa P, Ciaula AD, Bonfrate L, Wang DQ. Therapy of gallstone disease: What it was, what it is, what it will be. World journal of gastrointestinal pharmacology and therapeutics. Apr 6 2012;3(2):7-20.
Portincasa P, Di Ciaula A, Grattagliano I. Preventing a Mass Disease: The Case of Gallstones Disease: Role and Competence for Family Physicians. Korean journal of family medicine. Jul 2016;37(4):205-213.
Portincasa P, Moschetta A, Petruzzelli M, Palasciano G, Di Ciaula A, Pezzolla A. Gallstone disease: Symptoms and diagnosis of gallbladder stones. Best practice & research. Clinical gastroenterology. 2006;20(6):1017-1029.
Portincasa P, Wang DQ. Effect of Inhibition of Intestinal Cholesterol Absorption on the Prevention of Cholesterol Gallstone Formation. Medicinal chemistry (Shariqah (United Arab Emirates)). 2017;13(5):421-429.
Pozo MJ, Gomez-Pinilla PJ, Camello-Almaraz C, Martin-Cano FE, Pascua P, Rol MA, . . . Camello PJ. Melatonin, a potential therapeutic agent for smooth muscle-related pathological conditions and aging. Current medicinal chemistry. 2010;17(34):4150-4165.
Prasad PC, Gupta S, Kaushik N. To study serum iron levels in patients of gall bladder stone disease and to compare with healthy individuals. The Indian journal of surgery. Feb 2015;77(1):19-22.
Rangaswamy R, Singh CG, Singh HM, Punyabati P, Nyuwi KT. Impact of Biliary Calculi on the Liver. Journal of clinical and diagnostic research: JCDR. Apr 2017;11(4):Pc04-pc07.
Rasyid A, Lelo A. The effect of curcumin and placebo on human gall-bladder function: an ultrasound study. Alimentary pharmacology & therapeutics. Feb 1999;13(2):245-249.
Rasyid A, Rahman AR, Jaalam K, Lelo A. Effect of different curcumin dosages on human gall bladder. Asia Pacific journal of clinical nutrition. 2002;11(4):314-318.
Reddy RR, Srinivasan K. Dietary fenugreek and onion attenuate cholesterol gallstone formation in lithogenic diet-fed mice. International journal of experimental pathology. Oct 2011a;92(5):308-319.
Reddy RR, Srinivasan K. Effect of dietary fenugreek seeds on biliary proteins that influence nucleation of cholesterol crystals in bile. Steroids. Apr 2011b;76(5):455-463.
Resnick E, Shteingart S, Melamud B, Bdolah-Abram T, Zalut T, Reuben A, Lurie Y. Enzyme pattern of biliary colic: A counterintuitive picture. World journal of hepatology. Dec 28 2016;8(36):1629-1636.
Rohde U, Sonne DP, Christensen M, Hansen M, Bronden A, Torang S, . . . Knop FK. Cholecystokinin-Induced Gallbladder Emptying and Metformin Elicit Additive Glucagon-Like Peptide-1 Responses. The Journal of clinical endocrinology and metabolism. May 2016;101(5):2076-2083.
Romeu M, Aranda N, Giralt M, Ribot B, Nogues MR, Arija V. Diet, iron biomarkers and oxidative stress in a representative sample of Mediterranean population. Nutrition journal. Jul 16 2013;12:102.
Ros E. Health benefits of nut consumption. Nutrients. Jul 2010;2(7):652-682.
Rumsey S, Winders J, MacCormick AD. Diagnostic accuracy of Charcot's triad: a systematic review. ANZ journal of surgery. Apr 2017;87(4):232-238.
Saboor M, Zehra A, Qamar K, Moinuddin. Disorders associated with malabsorption of iron: A critical review. Pakistan journal of medical sciences. Nov-Dec 2015;31(6):1549-1553.
Sachdeva S, Khan Z, Ansari MA, Khalique N, Anees A. Lifestyle and gallstone disease: scope for primary prevention. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine. Oct 2011;36(4):263-267.
Sadr-Azodi O, Sanders DS, Murray JA, Ludvigsson JF. Patients with celiac disease have an increased risk for pancreatitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. Oct 2012;10(10):1136-1142.e1133.
Sakai Y, Tsuyuguchi T, Sugiyama H, Hayashi M, Senoo J, Kusakabe Y, . . . Yokosuka O. Comparison of endoscopic papillary balloon dilatation and endoscopic sphincterotomy for bile duct stones. World Journal of Gastrointestinal Endoscopy. May 25 2016;8(10):395-401.
Sang JH, Ki NK, Cho JH, Ahn JO, Sunwoo JG. Correlations between metabolic syndrome, serologic factors, and gallstones. Journal of physical therapy science. Aug 2016;28(8):2337-2341.
Sanikidze T, Chikvaidze E. Role of the Free Radicals in Mechanisms of Gallstone Formation: An EPR Study. Radiation protection dosimetry. Dec 2016;172(1-3):317-324.
Schwaitzberg SD, Roberts K, Romanelli JR, Desilets DJ, Earle D, Horgan S, . . . Kochman ML. The NOVEL trial: natural orifice versus laparoscopic cholecystectomy-a prospective, randomized evaluation. Surgical endoscopy. Dec 7 2017.
Seetharam P, Rodrigues G. Sphincter of Oddi and its dysfunction. Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association. Jan 2008;14(1):1-6.
Sekine K, Nagata N, Sakamoto K, Arai T, Shimbo T, Shinozaki M, . . . Uemura N. Abdominal visceral fat accumulation measured by computed tomography associated with an increased risk of gallstone disease. Journal of gastroenterology and hepatology. Aug 2015;30(8):1325-1331.
Setiawan VW, Pandol SJ, Porcel J, Wei PC, Wilkens LR, Le Marchand L, . . . Monroe KR. Dietary Factors Reduce Risk of Acute Pancreatitis in a Large Multiethnic Cohort. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. Feb 2017;15(2):257-265.e253.
Shabanzadeh DM, Jorgensen T, Linneberg A, Sorensen LT, Skaaby T. Vitamin D and gallstone disease-A population-based study. Endocrine. Dec 2016;54(3):818-825.
Shabanzadeh DM, Skaaby T, Sorensen LT, Eugen-Olsen J, Jorgensen T. Metabolic biomarkers and gallstone disease - a population-based study. Scandinavian journal of gastroenterology. Nov 2017;52(11):1270-1277.
Shabanzadeh DM, Skaaby T, Sorensen LT, Jorgensen T. Screen-detected gallstone disease and cardiovascular disease. European journal of epidemiology. Jun 2017;32(6):501-510.
Shabanzadeh DM, Sorensen LT, Jorgensen T. Determinants for clinical events in gallstone carriers unaware of their gallstones. Journal of gastroenterology and hepatology. Mar 2017a;32(3):721-726.
Shabanzadeh DM, Sorensen LT, Jorgensen T. Gallstone disease and mortality: a cohort study. International journal of public health. Apr 2017b;62(3):353-360.
Shaffer E. Cholelithiasis. Epocrates. https://online.epocrates.com/diseases/87311/Cholelithiasis/Key-Highlights. Last updated 1/12/2018. Accessed 01/24/2018.
Shan D, Fang Y, Ye Y, Liu J. EGCG reducing the susceptibility to cholesterol gallstone formation through the regulation of inflammation. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. Dec 2008;62(10):677-683.
Shiesh SC, Chen CY, Lin XZ, Liu ZA, Tsao HC. Melatonin prevents pigment gallstone formation induced by bile duct ligation in guinea pigs. Hepatology. Sep 2000;32(3):455-460.
Shirah BH, Shirah HA, Zafar SH, Albeladi KB. Clinical patterns of postcholecystectomy syndrome. Annals of hepato-biliary-pancreatic surgery. Feb 2018;22(1):52-57.
Shubha MC, Reddy RR, Srinivasan K. Antilithogenic influence of dietary capsaicin and curcumin during experimental induction of cholesterol gallstone in mice. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. Apr 2011;36(2):201-209.
Sies CW, Brooker J. Could these be gallstones? Lancet (London, England). Apr 16-22 2005;365(9468):1388.
Simic D, Milojevic I, Bogicevic D, Milenovic M, Radlovic V, Draskovic B, . . . Maksimovic R. Preventive effect of ursodeoxycholic acid on parenteral nutrition-associated liver disease in infants. Srpski arhiv za celokupno lekarstvo. Mar-Apr 2014;142(3-4):184-188.
Simon JA. Ascorbic acid and cholesterol gallstones. Medical hypotheses. Feb 1993;40(2):81-84.
Simon JA, Hudes ES. Serum ascorbic acid and gallbladder disease prevalence among US adults: the Third National Health and Nutrition Examination Survey (NHANES III). Archives of internal medicine. Apr 10 2000;160(7):931-936.
Simon JA, Hudes ES. Serum ascorbic acid and other correlates of gallbladder disease among US adults. American journal of public health. Aug 1998;88(8):1208-1212.
Simonsen MH, Erichsen R, Froslev T, Rungby J, Sorensen HT. Postmenopausal estrogen therapy and risk of gallstone disease: a population-based case-control study. Drug safety. Dec 2013;36(12):1189-1197.
Sinha R, Sharma N. Acute cholecystitis and laparoscopic cholecystectomy. JSLS : Journal of the Society of Laparoendoscopic Surgeons. Jan-Mar 2002;6(1):65-68.
Song XY, Xu S, Hu JF, Tang J, Chu SF, Liu H, . . . Chen NH. Piperine prevents cholesterol gallstones formation in mice. European journal of pharmacology. Mar 15 2015;751:112-117.
Srinivasan K. Anti-cholelithogenic potential of dietary spices and their bioactives. Critical reviews in food science and nutrition. May 24 2017;57(8):1749-1758.
Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and liver. Apr 2012;6(2):172-187.
Stokes CS, Gluud LL, Casper M, Lammert F. Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: a meta-analysis of randomized controlled trials. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. Jul 2014;12(7):1090-1100.e1092; quiz e1061.
Sulaberidze G, Okujava M, Liluashvili K, Tughushi M, Bezarashvili S. Dietary fiber's benefit for gallstone disease prevention during rapid weight loss in obese patients. Georgian medical news. Jun 2014(231):95-99.
Tanaja J, Meer JM. Cholelithiasis. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
Tarnasky PR. Post-cholecystectomy syndrome and sphincter of Oddi dysfunction: past, present and future. Expert review of gastroenterology & hepatology. Dec 2016;10(12):1359-1372.
Toouli J. Biliary Dyskinesia. Current treatment options in gastroenterology. Aug 2002;5(4):285-291.
Tsai CJ, Leitzmann MF, Hu FB, Willett WC, Giovannucci EL. Frequent nut consumption and decreased risk of cholecystectomy in women. The American journal of clinical nutrition. Jul 2004a;80(1):76-81.
Tsai CJ, Leitzmann MF, Hu FB, Willett WC, Giovannucci EL. A prospective cohort study of nut consumption and the risk of gallstone disease in men. American journal of epidemiology. Nov 15 2004b;160(10):961-968.
Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. Heme and non-heme iron consumption and risk of gallstone disease in men. The American journal of clinical nutrition. Feb 2007;85(2):518-522.
Turner AR, Bhimji SS. Ileus, Gallstone. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
Uhler ML, Marks JW, Voigt BJ, Judd HL. Comparison of the impact of transdermal versus oral estrogens on biliary markers of gallstone formation in postmenopausal women. The Journal of clinical endocrinology and metabolism. Feb 1998;83(2):410-414.
Upala S, Sanguankeo A, Jaruvongvanich V. Gallstone Disease and the Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Observational Studies. Scandinavian journal of surgery: SJS: official organ for the Finnish Surgical Society and the Scandinavian Surgical Society. Mar 2017;106(1):21-27.
Vassiliou MC, Laycock WS. Biliary dyskinesia. The Surgical clinics of North America. Dec 2008;88(6):1253-1272, viii-ix.
Vidyashankar S, Sambaiah K, Srinivasan K. Effect of dietary garlic and onion on biliary proteins and lipid peroxidation which influence cholesterol nucleation in bile. Steroids. Mar 2010a;75(3):272-281.
Vidyashankar S, Sambaiah K, Srinivasan K. Regression of preestablished cholesterol gallstones by dietary garlic and onion in experimental mice. Metabolism: clinical and experimental. Oct 2010b;59(10):1402-1412.
Vitek L, Carey MC. New pathophysiological concepts underlying pathogenesis of pigment gallstones. Clinics and research in hepatology and gastroenterology. Apr 2012;36(2):122-129.
Walcher T, Haenle MM, Kron M, Hay B, Mason RA, Walcher D, . . . Kratzer W. Vitamin C supplement use may protect against gallstones: an observational study on a randomly selected population. BMC gastroenterology. Oct 8 2009;9:74.
Walcher T, Haenle MM, Mason RA, Koenig W, Imhof A, Kratzer W. The effect of alcohol, tobacco and caffeine consumption and vegetarian diet on gallstone prevalence. European journal of gastroenterology & hepatology. Nov 2010;22(11):1345-1351.
Wang HH, Liu M, Li X, Portincasa P, Wang DQ. Impaired intestinal cholecystokinin secretion, a fascinating but overlooked link between coeliac disease and cholesterol gallstone disease. European journal of clinical investigation. Apr 2017;47(4):328-333.
Wang JK, Foster SM, Wolff BG. Incidental gallstones. The Permanente journal. Spring 2009;13(2):50-54.
Wang S, Wang Y, Xu J, Chen Y. Is the oral contraceptive or hormone replacement therapy a risk factor for cholelithiasis: A systematic review and meta-analysis. Medicine. Apr 2017;96(14).
Waniek S, di Giuseppe R, Esatbeyoglu T, Ratjen I, Enderle J, Jacobs G, . . . Lieb W. Association of Circulating Vitamin E (alpha- and gamma-Tocopherol) Levels with Gallstone Disease. Nutrients. Jan 27 2018;10(2).
Worthington HV, Hunt LP, McCloy RF, Maclennan I, Braganza JM. A pilot study of antioxidant intake in patients with cholesterol gallstones. Nutrition (Burbank, Los Angeles County, Calif.). Feb 1997;13(2):118-127.
Worthington HV, Hunt LP, McCloy RF, Ubbink JB, Braganza JM. Dietary antioxidant lack, impaired hepatic glutathione reserve, and cholesterol gallstones. Clinica chimica acta; international journal of clinical chemistry. Nov 2004;349(1-2):157-165.
Wybourn CA, Kitsis RM, Baker TA, Degner B, Sarker S, Luchette FA. Laparoscopic cholecystectomy for biliary dyskinesia: Which patients have long term benefit? Surgery. Oct 2013;154(4):761-767; discussion 767-768.
Yang F, Tang X, Ding L, Zhou Y, Yang Q, Gong J, . . . Yang L. Curcumin protects ANIT-induced cholestasis through signaling pathway of FXR-regulated bile acid and inflammation. Scientific reports. Sep 14 2016;6:33052.
Yu DD, Andrali SS, Li H, Lin M, Huang W, Forman BM. Novel FXR (farnesoid X receptor) modulators: Potential therapies for cholesterol gallstone disease. Bioorganic & medicinal chemistry. Sep 15 2016;24(18):3986-3993.
Zakko SF, Chopra S, Grover S. UpToDate: Patient Education: Gallstones (Beyond the Basics). Available at https://www.uptodate.com/contents/gallstones-beyond-the-basics. Last updated 02/21/2018. Accessed 03/14/2018.
Zhang XH, Andreotti G, Gao YT, Deng J, Liu E, Rashid A, . . . Hsing AW. Tea drinking and the risk of biliary tract cancers and biliary stones: a population-based case-control study in Shanghai, China. International journal of cancer. Jun 15 2006;118(12):3089-3094.
Zhang YP, Li WQ, Sun YL, Zhu RT, Wang WJ. Systematic review with meta-analysis: coffee consumption and the risk of gallstone disease. Alimentary pharmacology & therapeutics. Sep 2015;42(6):637-648.
Zheng Y, Xu M, Li Y, Hruby A, Rimm EB, Hu FB, . . . Qi L. Gallstones and Risk of Coronary Heart Disease: Prospective Analysis of 270 000 Men and Women From 3 US Cohorts and Meta-Analysis. Arteriosclerosis, thrombosis, and vascular biology. Sep 2016;36(9):1997-2003.
Zimmer V, Lammert F. Acute Bacterial Cholangitis. Viszeralmedizin. Jun 2015;31(3):166-172.
