Life Extension Magazine®
After decades of heightened sun-risk awareness, skin cancer is still the most common malignancy in the United States.1
About 87,000 new cases of melanoma will be diagnosed in the US in 2017. Nearly 10,000 Americans will die from metastatic melanoma.2
According to the latest report by the Environmental Working Group,3 almost 75% of sunscreens contain “worrisome ingredients” and offer inferior sun protection.
For example, 70% of the sunscreens evaluated still contain a compound that, when applied to the skin and exposed to sunlight, generates reactive oxygen species.3-5 This means that increased use of these sunscreens may be a factor in increased skin cancer rates!
Particularly surprising, some of the highest-SPF-rated sunscreens are often the riskiest.6
Game-changing sunscreen formulas have been developed that block the full spectrum of harmful ultraviolet radiation and provide plant extracts that inhibit and even reverse solar-induced skin damage.
The Escalating Skin Cancer Epidemic
One in every three diagnosed cancers is a skin malignancy.7
Over the past 40 years, melanoma cases have skyrocketed more than four-fold for men and more than eight-fold for women.8 Non-melanoma skin cancers affect over 3 million people.2 Depletion of the ozone layer has contributed to increased risk of skin cancer globally.7
Although melanoma is the least common form of skin cancer, it is the most deadly. Other skin cancers, while less dangerous, can involve costly surgical procedures to remove.9 To give you an idea of skin cancer prevalence, basal cell carcinoma is more common than all other human malignancies combined.10,11
These staggering rates underscore the fact that most sunscreens are failing to deliver adequate protection against damaging solar rays.12,13 Even more concerning are chemicals found in many sunscreens that appear to increase free radicals and deactivate antioxidant systems, which may contribute to skin cancer risk!3-5
It’s no wonder that skin cancer is the most common American cancer.1 Yet it remains one of the most preventable forms of the disease.14
Solar rays cause damage that goes beyond cancer. Sun-induced aging of the skin or photoaging is clinically characterized by deep wrinkles, mottled pigmentation, rough skin, skin-tone loss, dryness, spider veins, leathery appearance, loss of elasticity, and precancerous lesions.15,16
Photoaging occurs most frequently on sun-exposed areas such as the face, neck, upper chest, hands, and forearms.16
Only about 14% of men and 30% of women regularly wear sunscreen on their face and other exposed skin.17 Many people halfheartedly limit their sun exposure. But effective protection is needed every day, as solar rays damage skin far more than anyone realizes!
Failures of Commercial Sunscreens
A number of factors drive the exploding incidence of skin cancer cases. Armed with new sunscreen options, individuals can now get greater protection than ever before.
Most people skip wearing sunscreen on cloudy days. Radiation scattering by clouds, however, can produce higher total radiation on cloudy days than on sunny days. About 80% of ultraviolet light penetrates moderate cloud cover.18,19
Cloudy or not, most people don’t worry about sunscreen if they’re going to be outside for under an hour. But only a few minutes of daily exposure to ultraviolet photons can alter skin structure,20,21 leading to skin cancer and premature skin aging.
Even those who wear sunscreen daily generally apply it incorrectly and fail to reapply it regularly as required. Many consumers apply only 25%-50% of the recommended amount.22 And it’s still important to avoid unnecessary sun exposure even after proper sunscreen application.23,24
Consumers are fooled by a high and misleading “sun protection factor,” or SPF.
All SPF means is that these products block the UVB rays that affect the superficial epidermis skin layer.6,25 While this helps prevent sunburn, it does nothing to block the UVA radiation that makes up 95% of ultraviolet radiation and causes much greater damage.3,25
UVA penetrates more deeply—accelerating skin aging, suppressing immunity, and fostering skin cancer.26-28
Equally misleading are the labels on so-called “broad-spectrum” sunscreens that claim to block carcinogenic UVA radiation in addition to sunburn-causing UVB. The Environmental Working Group determined that only half of all sunscreens would offer enough UVA protection to be sold in Europe (which has much higher standards).29
Most frightening, the public is led to believe that higher SPF ratings are superior, but they give people a false sense of security. A 100 SPF provides just 1% more UV protection than a 50 SPF—although the higher rating encourages longer exposure.6
But any sunscreen will provide some cancer defense, right? Wrong. A 2016 review of sunscreen products found that almost three-fourths of the examined sunscreens contain “worrisome ingredients” that may increase cancer risk, thus defeating the purpose of using them. For example, 70% of the sunscreens evaluated in this report still contain a compound (oxybenzone) that, when applied to the skin and exposed to sunlight, generates reactive oxygen species (ROS).3-5
What You Need to Know
 |
Topical Protection against UV Radiation
- Skin cancer is the most common form of cancer in the US.
- Most sunscreens contain dangerous chemicals that can boost skin cancer risk.
- Next-generation sunscreen formulas safely block the full range of ultraviolet radiation using complementary UV-blocking compounds.
- This sunscreen’s second line of defense employs an array of botanicals that block and repair the skin-damaging effects of UV light that reaches the skin.
Blocking the Dangers of Ultraviolet Radiation
An effective sun-protection formulation needs to work on different levels, because skin damage itself occurs via multiple mechanisms.
In the skin, UV rays generate free radicals and other substances that damage the DNA.30 Ultraviolet light destroys Langerhans cells, specialized immune cells found abundantly in the skin that protect against invading pathogens and participate in the immune response against skin cancer.30-32 UV rays also contribute to the breakdown of collagen and elastin, which accelerates skin aging.33,34
Solar radiation-induced oxidative stress triggers the release of proinflammatory cytokines and growth factors, further damaging elastin and collagen and breaking down the skin’s structural integrity.35
Adding to the risks are some commercial sun protection products themselves.36 Found in most sunscreens, octibenzone and oxybenzone are rated “high-risk” by the Environmental Working Group.37
In a 2016 report, oxybenzone was still found in nearly 70% of sunscreens.3,37 And higher-SPF sunscreens generally contain higher concentrations of dangerous chemicals.6
Topical Lotion Protects against UV Damage

Science-based topical formulas are now available that safely block solar radiation—while adding a second line of defense against the destructive mechanisms of any UV light reaching the skin.
One of these new sunscreens can be found in a light lotion that readily absorbs into skin without a white, greasy mess. Health-conscious individuals should apply this formula daily, even on cloudy days, and reapply every two hours if you are remaining outdoors.
This new sunscreen lotion contains ingredients that safely block UV radiation and may reverse its DNA-damaging and photoaging effects. Unlike many commercial products, the ingredients in this new lotion formulation rate scores of between 1 and 3 on the hazard scale of the independent Environmental Working Group—a scale that rates “high hazard” chemicals as being between 7 and 10.
The new lotion formulation includes zinc oxide, which blocks both UVA2 and UVA1 rays. Although some products exclusively rely on zinc oxide to fight UVB, it provides incomplete UVB protection. Therefore, this new lotion also contains titanium dioxide, which more effectively reflects and blocks UVB and further blocks UVA2.38
Combining these two compounds means that just 6% concentrations of each are required. This avoids the white-smeary appearance of products containing only one of these compounds, which often discourages users from applying adequate amounts. Please know that titanium dioxide remains on your skin and is not systemically absorbed.
Convenient Spray Bottle Option
For convenient whole body application, a new sunscreen spray has been developed that provides similar benefits to the new lotion. Zinc oxide and titanium dioxide cannot be used in this formula because they will clog a spray bottle.
To accommodate a spray mist, scientists combined the following UV-blocking agents:
- Avobenzone to absorb UVA1 rays.38
- Octocrylene to filter out UVA2 and UVB.38,39
- Octisalate and homosalate to fully enhance UVB radiation defense.38
Most spray-on sun products are slow-drying, but this formulation contains just enough alcohol, allowing for instant drying and encouraging convenient reapplications throughout the day.
A review panel assessing this (FDA-approved40) alcohol found no evidence of phototoxicity on human skin, even at higher concentrations.41
By including different ingredient combinations, both the new lotion and spray provide unsurpassed protection against the full range of UVA radiation, as well as UVB.
Recent research on cancer-fighting plant compounds shows how combining botanical agents with UV-blocking compounds can inhibit and proactively repair damage that still occurs.
Few Sunscreens Can Block the Cancer-Causing Wavelengths of UV Radiation
 |
Different wavelengths of sunlight radiation represent different levels of risk:77
- UVA rays—wavelengths ranging from about 315 to 400 nanometers—were once thought to have minor skin effects. Studies now show that UVA penetrates skin much deeper than UVB.27 UVA makes up about 95% of the UV energy reaching the earth, with UVB comprising just 5%. UVA causes more severe skin damage.85 It is crucial to block UVA rays—and to prevent cellular damage done by UVA rays that get through. The innovative lotion described in this article filters out UVA by combining zinc oxide and titanium dioxide, while the spray version blocks UVA with a combination of avobenzone and octocrylene.38 Neither formula contains the risky compounds found in most sunscreens.3 Both formats safely block UV radiation and may reverse its DNA damaging and photoaging effects. They do so with an array of safe botanical extracts shown in studies to naturally inhibit and help reverse these effects at the cellular level. These extracts include a novel oat beta-glucan, green tea, licorice, milk thistle, and rosemary.
- UVB rays—wavelengths which range from 280 to about 315 nanometers and which are strongest around midday—affect the superficial layer of the skin known as the epidermis and cause sunburn. The novel lotion formulation described in this article safely and effectively blocks UVB by combining zinc oxide and titanium dioxide, while the spray formulation accomplishes the same by combining octisalate, homosalate, and octocrylene.38 The risky compounds found in most sunscreens3 have been completely excluded.
- UVC rays—wavelengths which range from 100 to 280 nanometers—are almost completely absorbed by the ozone layer and do not affect the skin.
Oat Beta-Glucans Help Reverse Wrinkling
Oat beta-glucans have been shown to rapidly and deeply permeate the epidermis.42,43
Deep in the skin they activate genes that enhance collagen synthesis and promote skin cell-repair.44 Clinical research shows that beta-glucans restructure human tissue, significantly reversing wrinkling.43
Published in Phytotherapy Research in 2014, a review concluded that beta-glucans strengthen the skin’s ability to inhibit environmentally-triggered aging/wrinkling.45
Green Tea Extract Enhances DNA Repair
Topical green tea extract and its polyphenol epigallocatechin-3-gallate (EGCG) were shown to prevent skin cancer in lab animals.
Green tea extract and EGCG enhances DNA repair and maintains robust immune function. It counters UV radiation’s effects, which invariably suppress immune function and promote UV-induced skin cancers.46-49
Green tea-treated skin has shown reduced sunburn cell numbers, less depletion of epidermal Langerhans cells, and photoprotective effects against UVA. Adding green tea extract to sunscreens may help thwart skin cancer at multiple stages in its development.46-49
Beyond cancer, studies show that green tea and green tea extract prevent photoaging when used orally or topically.50-54 A lab study demonstrated that topically applied green tea polyphenols have clearly greater photoprotective efficacy than when taken orally.46
In 2015, a review of previous studies concluded that green tea polyphenols:
“…protect against UV irradiation-stimulated skin photoaging” and inhibit its hyperpigmentation, wrinkling, and immunosuppression.55
Licorice Root Extract Suppresses Skin Inflammation
Licorice root has been recognized in Chinese medicine for its anti-inflammatory, antiviral, anti-ulcer, and cancer-preventive properties.56 Licorice has been used medicinally since prehistoric times.57 Studies now show that licorice constituents inhibit the growth of melanoma cancer cells and induce many cancer cell types to undergo apoptosis (programmed cell death).58,59
A double-blind study concluded that licorice extract is potentially effective for treating atopic dermatitis—a chronic, inflammatory skin disease.60 Two years later, a second group of researchers found that the licorice constituent glycyrrhizin “might offer protection from the damage induced in humans by UVB radiation.”61
Milk Thistle Extract Blocks DNA Damage
Milk thistle compounds—silibinin and silymarin—deliver potent antioxidant, anti-inflammatory, and immune-enhancing properties.62-67 Significant decreases in skin cancer number and size were shown for topical application of silymarin and silibinin.66,67
Specifically investigating UV radiation, scientists found that silibinin blocks DNA skin damage and impedes cancer cell growth in mice.67 It may do this in part by enhancing the activity of the p53 gene, which protects against cancer.62 Compellingly, researchers found that silibinin helps repair DNA damage caused by previous exposure to UVB radiation.68
Silymarin was also shown to protect against skin-tumor promotion.66 One investigation concluded that silymarin “may favorably supplement sunscreen protection and provide additional anti-photocarcinogenic protection.”62
Rosemary Extract Inhibits Skin Tumor Growth

Rosemary has been shown to enhance the body’s ability to eliminate potential carcinogens.69 Lab studies have shown that rosemary slows or stops DNA damage and tumor-cell proliferation, induces tumor-cell apoptosis, and suppresses genes that enable tissue invasion and metastatic spread.70-72 Two rosemary compounds—carnosic and ursolic acids—particularly benefit the skin.73-75
In a similar study relevant to sunscreens, topically applied rosemary extract inhibited tumor growth—up to 99%, depending on concentration!73
Ursolic acid found in rosemary inhibits reactive oxygen species in skin cells and prevents the skin-aging effects of UVA rays.76 Remarkably, ursolic acid also powerfully blocks the growth of cancerous melanoma cells.75
Plant Extracts Inhibit UV Skin Damage
Oat kernel extract has been clinically demonstrated to regenerate skin.43
Green tea, licorice, milk thistle, and rosemary, have been shown to deliver potent radical-scavenging, anti-inflammatory, anticancer, and DNA-protective effects.
These properties are important when seeking to inhibit and repair skin damage by UV radiation.46-49,58,59,67,76 A published study that evaluated these plant extracts concluded that:
“…botanicals may favorably supplement sunscreen protection and may provide additional antiphotocarcinogenic protection, including the protection against other skin disorders caused by solar UV radiation.”12
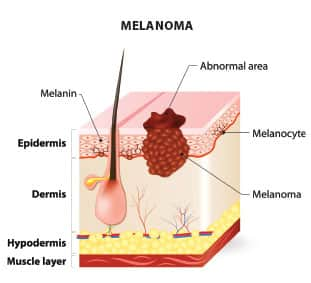
Deadly Melanoma Can Occur Anywhere in the Body
 |
Melanoma develops from pigment-containing skin cells called melanocytes. Exposure to ultraviolet radiation is considered a major risk factor, and possibly a cause, of melanoma.78-80
Unrepaired DNA damage to skin cells triggers mutations that lead the cells to multiply rapidly and form malignant tumors.81 There is a common misconception that melanoma only affects the skin, but it can occur anywhere there are melanocytes, including on mucosal surfaces.82
While this deadly cancer is typically diagnosed in the skin, melanoma also occurs in the mouth, nose, eye, and various body organs. Ocular melanoma is the most common eye cancer.82
A particularly dangerous area where melanoma lesions can form is the scalp underneath the hair.83 Often obscured, non-surface melanomas are usually far advanced by the time they’re diagnosed. Gastrointestinal tract melanomas often represent metastasized melanoma.84
Melanoma cells are highly malignant and tend to be aggressive, with a tendency to metastasize.85,86 Metastatic melanoma has a poor prognosis.87 Although melanoma accounts for only 4% of all skin cancer cases, it is responsible for the greatest number of skin cancer-related deaths.88
Summary
Skin cancer is the most common malignancy in the United States, yet most people are not properly guarding against the damaging impact of UV radiation.
Many commercial sunscreens fail to provide adequate protection against UV radiation and contain potentially harmful chemicals that may boost skin cancer risk.
Novel sunscreen formulas safely block the full range of cancer-causing ultraviolet radiation.
Furthermore, they deliver botanicals that work at the cellular level to block and repair the damage inflicted by UV rays and normal aging.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Available at: https://www.cdc.gov/cancer/skin/statistics/. Accessed February 14, 2017.
- Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Accessed February 14, 2017.
- Available at: http://www.ewg.org/sunscreen/report/executive-summary/. Accessed February 15, 2017.
- Schallreuter KU, Wood JM, Farwell DW, et al. Oxybenzone oxidation following solar irradiation of skin: photoprotection versus antioxidant inactivation. J Invest Dermatol. 1996;106(3):583-6.
- Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006;41(8):1205-12.
- Available at: http://www.ewg.org/sunscreen/report/whats-wrong-with-high-spf/. Accessed February 15, 2017.
- Available at: http://www.who.int/uv/faq/skincancer/en/index1.html. Accessed February 15, 2017.
- Reed KB, Brewer JD, Lohse CM, et al. Increasing incidence of melanoma among young adults: an epidemiological study in Olmsted County, Minnesota. Mayo Clin Proc. 2012;87(4):328-34.
- Dubas LE, Ingraffea A. Nonmelanoma skin cancer. Facial Plast Surg Clin North Am. 2013;21(1):43-53.
- Mohan SV, Chang AL. Advanced Basal Cell Carcinoma: Epidemiology and Therapeutic Innovations. Curr Dermatol Rep. 2014;3:40-5.
- Chung S. Basal cell carcinoma. Arch Plast Surg. 2012;39(2):166-70.
- Baliga MS, Katiyar SK. Chemoprevention of photocarcinogenesis by selected dietary botanicals. Photochem Photobiol Sci. 2006;5(2):243-53.
- Haywood R, Wardman P, Sanders R, et al. Sunscreens inadequately protect against ultraviolet-A-induced free radicals in skin: implications for skin aging and melanoma? J Invest Dermatol. 2003;121(4):862-8.
- Available at: https://www.ncbi.nlm.nih.gov/books/NBK247164/. Accessed February 17, 2017.
- Yaar M, Eller MS, Gilchrest BA. Fifty years of skin aging. J Investig Dermatol Symp Proc. 2002;7(1):51-8.
- Helfrich YR, Sachs DL, Voorhees JJ. Overview of skin aging and hotoaging. Dermatol Nurs. 2008;20(3):177-83; quiz 84.
- Available at: https://www.aad.org/media/news-releases/study-most-americans-don-t-use-sunscreen. Accessed February 17, 2017.
- Available at: http://www.who.int/uv/resources/archives/fs271/en/. Accessed February 20, 2017.
- Available at: http://www.skincancer.org/prevention/sun-protection/sunscreen/the-skin-cancer-foundations-guide-to-sunscreens. Accessed February 20, 2017.
- Fisher GJ, Datta SC, Talwar HS, et al. Molecular basis of sun-induced premature skin ageing and retinoid antagonism. Nature. 1996;379(6563):335-9.
- Biniek K, Levi K, Dauskardt RH. Solar UV radiation reduces the barrier function of human skin. Proc Natl Acad Sci U S A. 012;109(42):17111-6.
- Available at: https://www.aad.org/media/stats/prevention-and-care/sunscreen-faqs. Accessed February 20, 2017.
- Wang SQ, Dusza SW. Assessment of sunscreen knowledge: a pilot survey. Br J Dermatol. 2009;161 Suppl 3:28-32.
- Available at: https://www.ncbi.nlm.nih.gov/books/NBK247163/. Accessed February 20, 2017.
- Pandel R, Poljsak B, Godic A, et al. Skin photoaging and the role of antioxidants in its prevention. ISRN Dermatol. 2013;2013:930164.
- Available at: http://www.who.int/uv/faq/uvhealtfac/en/. Accessed February 20, 2017.
- Available at: http://www.skincancer.org/prevention/uva-and-uvb. Accessed February 20, 2017.
- Schwarz T. Ultraviolet radiation--immune response. J Dtsch Dermatol Ges. 2005;3 Suppl 2:S11-8.
- Available at: http://www.ewg.org/release/Sunscreens-Get-Flunking-Grade-for-UVA-Protection. Accessed February 15, 2017.
- Lee CH, Wu SB, Hong CH, et al. Molecular Mechanisms of UV-Induced Apoptosis and Its Effects on Skin Residential Cells: The Implication in UV-Based Phototherapy. Int J Mol Sci. 2013;14(3):6414-35.
- Kolgen W, Both H, van Weelden H, et al. Epidermal langerhans cell depletion after artificial ultraviolet B irradiation of human skin in vivo: apoptosis versus migration. J Invest Dermatol. 2002;118(5):812-7.
- Nakano T, Oka K, Sugita T, et al. Antitumor activity of Langerhans cells in radiation therapy for cervical cancer and its modulation with SPG administration. In Vivo. 1993;7(3):257-63.
- Gueranger Q, Li F, Peacock M, et al. Protein oxidation and DNA repair inhibition by 6-thioguanine and UVA radiation. J Invest Dermatol. 2014;134(5):1408-17.
- Schweikert K, Gafner F, Dell’Acqua G. A bioactive complex to protect proteins from UV-induced oxidation in human epidermis. Int J Cosmet Sci. 2010;32(1):29-34.
- Chen L, Hu JY, Wang SQ. The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67(5):1013-24.
- Available at: http://monographs.iarc.fr/ENG/Monographs/vol55/mono55.pdf. Accessed February 20, 2017.
- Available at: http://www.ewg.org/sunscreen/report/the-trouble-with-sunscreen-chemicals/. Accessed February 20, 2017.
- Available at: http://www.skinacea.com/sunscreen/uv-filters-chart.html#.Voj3MO9Iiob. Accessed February 21, 2017.
- Available at: http://www.smartskincare.com/skinprotection/sunblocks/sunblock_octocylene.html. Accessed February 21, 2017.
- Available at: https://www.fda.gov/Cosmetics/Labeling/Claims/ucm2005201.htm. Accessed February 21, 2017.
- Cosmetic Ingredient Review Expert Panel. Final report of the safety assessment of Alcohol Denat., including SD Alcohol 3-A, SD Alcohol 30, SD Alcohol 39, SD Alcohol 39-B, SD Alcohol 39-C, SD Alcohol 40, SD Alcohol 40-B, and SD Alcohol 40-C, and the denaturants, Quassin, Brucine Sulfate/Brucine, and Denatonium Benzoate. Int J Toxicol. 2008;27 Suppl 1:1-43.
- Meyer W, Schonnagel B, Fleischer LG. A note on integumental (1-->3)(1-->6)beta-D-glucan permeation, using the porcine ear skin model. J Cosmet Dermatol. 2006;5(2):130-4.
- Pillai R, Redmond M, Röding J. Anti-Wrinkle Therapy: Significant New Findings in the Non-Invasive Cosmetic Treatment of Skin Wrinkles with Beta-Glucan. Int J Cosmet Sci. 2005;27(5):292.
- Wei D, Zhang L, Williams DL, et al. Glucan stimulates human dermal fibroblast collagen biosynthesis through a nuclear factor-1 dependent mechanism. Wound Repair Regen. 2002;10(3):161-8.
- Du B, Bian Z, Xu B. Skin health promotion effects of natural beta-glucan derived from cereals and microorganisms: a review. Phytother Res. 2014;28(2):159-66.
- Vayalil PK, Elmets CA, Katiyar SK. Treatment of green tea polyphenols in hydrophilic cream prevents UVB-induced oxidation of lipids and proteins, depletion of antioxidant enzymes and phosphorylation of MAPK proteins in SKH-1 hairless mouse skin. Carcinogenesis. 2003;24(5):927-36.
- Chung JH, Han JH, Hwang EJ, et al. Dual mechanisms of green tea extract (EGCG)-induced cell survival in human epidermal keratinocytes. Faseb j. 2003;17(13):1913-5.
- Katiyar SK. Skin photoprotection by green tea: antioxidant and immunomodulatory effects. Curr Drug Targets Immune Endocr Metabol Disord. 2003;3(3):234-42.
- Chiu A, Kimball AB. Topical vitamins, minerals and botanical ingredients as modulators of environmental and chronological skin damage. Br J Dermatol. 2003;149(4):681-91.
- Katiyar S, Elmets CA, Katiyar SK. Green tea and skin cancer: photoimmunology, angiogenesis and DNA repair. J Nutr Biochem. 2007;18(5):287-96.
- Elmets CA, Singh D, Tubesing K, et al. Cutaneous photoprotection from ultraviolet injury by green tea polyphenols. J Am Acad Dermatol. 2001;44(3):425-32.
- Rees JR, Stukel TA, Perry AE, et al. Tea consumption and basal cell and squamous cell skin cancer: results of a case-control study. J Am Acad Dermatol. 2007;56(5):781-5.
- Chiu AE, Chan JL, Kern DG, et al. Double-blinded, placebo-controlled trial of green tea extracts in the clinical and histologic appearance of photoaging skin. Dermatol Surg. 2005;31(7 Pt 2):855-60; discussion 60.
- Song XZ, Xia JP, Bi ZG. Effects of (-)-epigallocatechin-3-gallate on expression of matrix metalloproteinase-1 and tissue inhibitor of metalloproteinase-1 in fibroblasts irradiated with ultraviolet A. Chin Med J (Engl). 2004;117(12):1838-41.
- Roh E, Kim JE, Kwon JY, et al. Molecular mechanisms of green tea polyphenols with protective effects against skin photoaging. Crit Rev Food Sci Nutr. 2017;57(8):1631-7.
- Wang ZY, Nixon DW. Licorice and cancer. Nutr Cancer. 2001;39(1):1-11.
- Fiore C, Eisenhut M, Ragazzi E, et al. A history of the therapeutic use of liquorice in Europe. J Ethnopharmacol. 2005;99(3):317-24.
- Song NR, Lee E, Byun S, et al. Isoangustone A, a novel licorice compound, inhibits cell proliferation by targeting PI3K, MKK4, and MKK7 in human melanoma. Cancer Prev Res (Phila). 2013;6(12):1293-303.
- Hibasami H, Iwase H, Yoshioka K, et al. Glycyrrhetic acid (a metabolic substance and aglycon of glycyrrhizin) induces apoptosis in human hepatoma, promyelotic leukemia and stomach cancer cells. Int J Mol Med. 2006;17(2):215-9.
- Saeedi M, Morteza-Semnani K, Ghoreishi MR. The treatment of atopic dermatitis with licorice gel. J Dermatolog Treat. 2003;14(3):153-7.
- Rossi T, Benassi L, Magnoni C, et al. Effects of glycyrrhizin on UVB-irradiated melanoma cells. In Vivo. 2005;19(1):319-22.
- Katiyar SK. Silymarin and skin cancer prevention: anti-inflammatory, antioxidant and immunomodulatory effects (Review). Int J Oncol. 2005;26(1):169-76.
- Gazak R, Walterova D, Kren V. Silybin and silymarin--new and emerging applications in medicine. Curr Med Chem. 2007;14(3):315-38.
- Svobodova A, Zdarilova A, Maliskova J, et al. Attenuation of UVA-induced damage to human keratinocytes by silymarin. J Dermatol Sci. 2007;46(1):21-30.
- Wright TI, Spencer JM, Flowers FP. Chemoprevention of nonmelanoma skin cancer. J Am Acad Dermatol. 2006;54(6):933-46; quiz 47-50.
- Lahiri-Chatterjee M, Katiyar SK, Mohan RR, et al. A flavonoid antioxidant, silymarin, affords exceptionally high protection against tumor promotion in the SENCAR mouse skin tumorigenesis model. Cancer Res. 1999;59(3):622-32.
- Mallikarjuna G, Dhanalakshmi S, Singh RP, et al. Silibinin protects against photocarcinogenesis via modulation of cell cycle regulators, mitogen-activated protein kinases, and Akt signaling. Cancer Res. 2004;64(17):6349-56.
- Singh RP, Agarwal R. Mechanisms and preclinical efficacy of silibinin in preventing skin cancer. Eur J Cancer. 2005;41(13):1969-79.
- Tsai CW, Lin CY, Wang YJ. Carnosic acid induces the NAD(P)H: quinone oxidoreductase 1 expression in rat clone 9 cells through the p38/nuclear factor erythroid-2 related factor 2 pathway. J Nutr. 2011;141(12):2119-25.
- Slamenova D, Kuboskova K, Horvathova E, et al. Rosemary-stimulated reduction of DNA strand breaks and FPG-sensitive sites in mammalian cells treated with H2O2 or visible light-excited Methylene Blue. Cancer Lett. 2002;177(2):145-53.
- Kar S, Palit S, Ball WB, et al. Carnosic acid modulates Akt/IKK/NF-kappaB signaling by PP2A and induces intrinsic and extrinsic pathway mediated apoptosis in human prostate carcinoma PC-3 cells. Apoptosis. 2012;17(7):735-47.
- Yesil-Celiktas O, Sevimli C, Bedir E, et al. Inhibitory effects of rosemary extracts, carnosic acid and rosmarinic acid on the growth of various human cancer cell lines. Plant Foods Hum Nutr. 2010;65(2):158-63.
- Huang MT, Ho CT, Wang ZY, et al. Inhibition of skin tumorigenesis by rosemary and its constituents carnosol and ursolic acid. Cancer Res. 1994;54(3):701-8.
- Offord EA, Gautier JC, Avanti O, et al. Photoprotective potential of lycopene, beta-carotene, vitamin E, vitamin C and carnosic acid in UVA-irradiated human skin fibroblasts. Free Radic Biol Med. 2002;32(12):1293-303.
- Harmand PO, Duval R, Delage C, et al. Ursolic acid induces apoptosis through mitochondrial intrinsic pathway and caspase-3 activation in M4Beu melanoma cells. Int J Cancer. 2005;114(1):1-11.
- Soo Lee Y, Jin DQ, Beak SM, et al. Inhibition of ultraviolet-A-modulated signaling pathways by asiatic acid and ursolic acid in HaCaT human keratinocytes. Eur J Pharmacol. 2003;476(3):173-8.
- Available at: https://ntp.niehs.nih.gov/ntp/newhomeroc/roc10/uv_no_appendices_508.pdf. Accessed February 21, 2017.
- Available at: https://www.cancer.org/cancer/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html. Accessed March 21, 2017.
- Available at: http://www.skincancer.org/skin-cancer-information/melanoma. Accessed March 21, 2017.
- Available at: http://www.mayoclinic.org/diseases-conditions/melanoma/basics/definition/con-20026009. Accessed March 21, 2017.
- Available at: http://www.skincancer.org/healthy-lifestyle/anti-aging/seniors. Accessed February 22, 2017.
- Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0032516/. Accessed February 22, 2017.
- Available at: http://www.skincancer.org/true-stories/haircut. Accessed February 22, 2017.
- Liang KV, Sanderson SO, Nowakowski GS, et al. Metastatic malignant melanoma of the gastrointestinal tract. Mayo Clin Proc. 2006;81(4):511-6.
- Available at: https://www.melanoma.org/understand-melanoma/what-is-melanoma/metastatic-melanoma. Accessed March 21, 2017.
- Tas F. Metastatic behavior in melanoma: timing, pattern, survival, and influencing factors. J Oncol. 2012;2012:647684.
- Available at: https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html. Accessed March 21, 2017.
- Available at: http://my.clevelandclinic.org/health/articles/the-facts-about-melanoma. Accessed February 22, 2017.

