Life Extension Magazine®
How To Prevent Breast Cancer |
|
In 1971 when President Richard Nixon declared "war on cancer" the chance of a woman getting breast cancer over her lifetime was 1 in 20, which was up from 1 in 30 in 1960. Today--after hundreds of millions of dollars of research money spent fighting the disease--the odds are now a shocking 1 in 8. Every three minutes, a woman in the United States is diagnosed with breast cancer; every 12 minutes a woman dies from it. According to the American Cancer Society, more than 180,000 women will be diagnosed with breast cancer in the coming year, and about 46,000 women will die from it. Breast cancer has become the second largest cause of cancer deaths in women (next to lung cancer), and the leading cause of death for women between 35 and 54. Ever since the "war on cancer" was declared, more women have died of breast cancer than the total number of Americans who lost their lives in World War I & II, the Korean war, and the Vietnam war combined! The Campaign For Earlier Diagnosis Of Breast CancerThe escalating breast cancer rate (1.8% per year since 1973) has occurred in spite of major efforts in the past 24 years by the government and the American Cancer Society to convince women to go in for regular mammograms and to perform more frequent self breast examinations. The purpose of this massive propaganda campaign has been to promote the early diagnosis of breast cancer in an effort to increase the odds of curing the disease. The result of this campaign has been a substantial increase in the use of mammography. Only a small decrease in mortality from breast cancer has been observed, which has been insufficient to stem the tide of the increasing incidence of the disease. It is responsible for killing middle-aged women at an unprecedented rate, and striking terror into the hearts of women of all ages! The Failure Of The Medical Establishment In the face of the vast, rapidly-growing number of women who have been mutilated, made ill, and died as a result of the breast cancer epidemic tens of millions of women who live in abject terror that they may soon become victims of this horrific disease. The behavior of the medical establishment has been pitiful and absolutely appalling! In spite of new and exciting alternatives for the treatment of breast cancer, the establishment has refused to budge from its exclusive use of surgery, radiation and chemotherapy to treat women with breast cancer. Although these modalities cause severe pain, disfigurement, and terrible illness with only a modest "cure" rate, very few oncologists have even considered the use of alternative immune-system-boosting cancer therapies. Even more shocking, however, has been the failure of the establishment to consider the prevention of breast cancer, which is a far better alternative than any type of treatment. This utter abdication of moral and medical responsibility has come in the face of a vast and rapidly growing body of scientific evidence that every woman can reduce her risk of breast cancer significantly! At the Life Extension Foundation, we never give up on any of our members, no matter how sick or close to death they may be. We've presented vital, Potentially lifesaving Information about innovative new treatments for cancer (including breast cancer) in past issues of Life Extension Magazine, and we will continue to do so in the future. In this issue of the magazine, however, we focus on the critical issue of preventing breast cancer. The Information and advice in this article has been derived in part from a new book on the subject: How To Prevent Breast Cancer by Ross Pelton, Ph.D., Taffy Clarke Pelton, M.A., and Vinton C. Vint M.D. |
How To Prevent Breast Cancer Estrogen Replacement Therapy: What's A Woman To Do?
|
||
One of the likely reasons for the increased incidence of breast cancer in the U.S. in recent years has been the increasing number of women who have been taking supplemental estrogen to replace the estrogen lost during and after menopause. Although estrogen replacement therapy (ERT) can eliminate the negative effects of the menopause (including hot flashes, sweats, headaches, and nervousness), and is effective in preventing osteoporosis (bone loss), heart attacks, and (perhaps) colon cancer, it also increases the risk of endometrial (uterine) cancer, ovarian cancer, and breast cancer. What Is The True Risk Of Breast Cancer?At the Life Extension Foundation, we've taken the position that ERT causes breast cancer for years because of the laboratory studies showing that estrogen is a growth hormone that induces cellular growth, which, under certain circumstances, can lead to the uncontrolled cell proliferation that occurs in malignant tumors. Short-Term Vs. Long-Term StudiesSome short-term studies have shown that estrogen does not cause cancer. However, in those studies in which women taking estrogen and/or a synthetic progestin were followed for more than ten years, there appears to be a significantly elevated risk of breast and ovarian cancer (and uterine cancer in women taking estrogen alone). The Life Extension Foundation bases its warning about the carcinogenic risk of estrogen and estrogen/progestin replacement therapies on these longer term studies. Elevated Risk Of Ovarian CancerAll the hoopla over The New England Journal's report about the elevated risk of breast cancer from estrogen replacement therapy obscured another report in the American Journal of Epidemiology, showing that long-term estrogen therapy increased the risk of fatal ovarian cancer. This 7-year study included 240,073 peri- and postmenopausal women. After adjusting for other risk factors, women who used estrogen for 6-8 years had a 40"% higher risk of fatal ovarian cancer, and women who used estrogen for 11 or more years had a 70% higher risk of fatal ovarian cancer!
The Estrogen DilemmaEstrogens are steroid hormones that promote youthful cellular division, and regrowth of cellular components in target organs of the body, including the brain. Too much estrogen increases the risk of cancer, yet estrogen is an important antiaging hormone that provides us with many health benefits. This creates a dilemma that conventional medicine has yet to resolve.
|
The Most popular Drug In The Country | |||||||||
| The most popular prescription drug in the United States is Premarin, which contains several types of natural estrogen derived from the urine of pregnant mares. Provera is the name of a popular synthetic progestin that is commonly taken with Premarin to prevent estrogen-induced uterine cancer, but it does not prevent estrogen-induced breast cancer. It is important to note that dangerous forms of estrogen can be produced naturally in the body, so avoiding FDA approved drugs like Premarin (which is a natural product) does not necessarily protect you against estrogen-induced cancer. The mechanisms by which estrogen causes cancer are well documented in the scientific literature. Yet, the profits generated by Premarin sales have enabled its manufacturer to create the impression that Premarin is the only estrogen replacement therapy for menopausal and postmenopausal women. Despite the medical establishment's enthusiastic endorsement, Premarin is not for everyone. According to a 1987 survey, more than 50% of women quit estrogen therapy after a year because of side effects or because they were concerned about its long-term cancer risks. On the other hand, many women feel wonderful on Premarin and plan to take it for the rest of their lives. The Life Extension Foundation has an alternative approach for women who are afraid of the cancer risks of long-term therapy with Premarin, or who cannot tolerate its side effects. Forms of EstrogenThe primary forms of estrogen are:
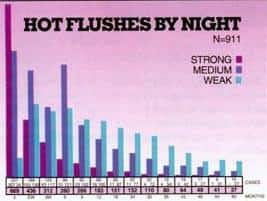
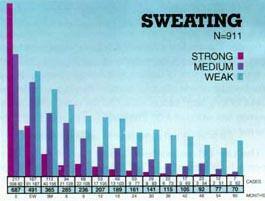
Estradiol and estrone are potent estrogens that are vulnerable to mutation. They are the estrogens that increase your risk of breast cancer. Estriol, on the other hand, is a weak estrogen that provides anti-aging benefits, without any apparent risk of breast cancer. Estradiol is the prime or true ovarian estrogen secreted by the ovary. Estrone is an estrogen that is synthesized from androstenedione or estradiol. While a small amount of estriol is produced by the ovary, most of the estriol found in the body is converted in the liver from estrone and by a more circuitous route from estradiol. During pregnancy, huge amounts of estriol are secreted by the placenta to protect the fetus. The urinary assay of estriol is used to assess the viability of the fetus. Estriol is used extensively in Europe for estrogen replacement therapy in menopausal and post menopausal women, but is rarely used for that purpose in the United States. Here is some of the evidence that estriol is appropriate for estrogen replacement therapy. Estriol Replacement TherapySince estriol is a weak estrogen, larger amounts must be used for estrogen replacement therapy. Estriol is used in doses of 2-to-8 mg. per day. A dose of 2-to-4 mg/day of estriol is equivalent to, and as effective as, 0.6-to-1.25 mg. of conjugated estrogens (Premarin) or estrone. One of the most common side effects of standard estrogen therapy (Premarin), when used without a progestin, is endometrial hyperplasia, or hyper-proliferation of the cells of the uterine lining, a condition which often turns into uterine cancer. Most investigators have found that estriol therapy, even at the high dose of 8 mg. per day, does not cause endometrial hyperplasia. In one study by scientists at the Medical College of Georgia in Augusta, 52 women with severe menopausal symptoms were given estriol succinate continuously for six months in doses of 2-to-8 mg/day. Results of StudySignificant improvements in symptoms were noted within one month of the start of the study, and they persisted as long as estriol therapy was continued. The degree of symptom improvement was directly related to the dose. Symptom relief was moderate at 2 mg/day, but marked at 8 mg/day. Estriol therapy also reversed vaginal atrophy and improved the quality of cervical mucus. No breakthrough bleeding occurred in any of the subjects and endometrial biopsies failed to show endometrial hyperplasia in any case, regardless of the dose of estriol used. They concluded that: "Estriol therapy may be employed in dosages up to 8 mg/day continuously, especially in those patients in whom other estrogens induce undesired side effects such as nausea, breakthrough bleeding or endometrial hyperplasia, and the recurrence of hot flushes during cyclic therapy of more potent estrogens. Because of these features, estriol deserves a place in our therapeutic resources. Being a weak estrogen, it does not induce endometrial proliferation or breakthrough bleeding of any consequence, while modifying menopausal symptoms. "A longer-term and larger prospective study of estriol therapy for the symptoms of the menopause was conducted by C. Lauritzen at the University of Ulm in Germany in the mid 1980s. A total of 911 patients with severe menopausal symptoms were given 2-8 mg/day of estriol succinate by 22 gynecologists at 11 hospitals in Germany for up to five years. The mean duration of the study was 2.2 years, with 121 of the patients (13.5%) receiving treatment over the entire five years of the study.
| |||||||||
Preventing Bone Loss |
|||||||||||||||||||
|
One of the major benefits of estrogen therapy is prevention of the bone loss associated with osteoporosis. Postmenopausal women taking estrogen experience 50% fewer bone fractures than women of comparable age who have not taken estrogen. Although no studies have yet been conducted in the U.S. to determine if estriol therapy can prevent osteoporosis, a prospective, double-blind study was recently completed in 136 postmenopausal women at the Chinese Great Wall Hospital in Beijing, China with Nylestriol (CEE,), a long-acting, estriol derivative that is metabolized into ethynyl estriol and estriol within the body. The subjects took 2 mg. of CEE, or placebo every day for up to a year, with measurements of forearm bone mass and lipoprotein levels performed every 3 months until the end of the study. They found significantly greater loss of bone mass and higher low-density lipoprotein levels in the placebo group. The authors concluded that: "CEE, is an effective estrogen for preventing bone loss and lipid disorders in postmenopausal women just as the most popular conjugated estrogen (Premarin), but is more convenient. Long-term CEE, medication, its effects on endometrium and the regimen of progestin combination await further study. " The most recent study with estriol therapy was conducted by gynecologists at the Veterans General Hospital Tapei in Taiwan. They gave 20 patients, age 44-62, who had undergone either natural or surgical menopause, 2 mg/day of estriol succinate for 2 years. They found that "estriol was very effective in improving major subjective climacteric complaints in 85% of patients, especially hot flushes and insomnia... The atrophic genital changes caused by estrogen deficiency also improved satisfactorily." Estriol Intravaginal CreamFurther evidence that estriol is effective in counteracting the symptoms of the menopause comes from studies with estriol intravaginal creams. One such study, conducted by scientists from the Technion Faculty of Medicine in Haifa, Israel, looked at urinary tract infections, a common affliction in post-menopausal women who suffer from an atrophying vagina characterized by elevated pH and a disrupted flora caused by lack of estrogen. In this study, 93 postmenopausal women with a history of recurrent urinary tract infections were enrolled in a randomized, double-blind trial of a topically applied intravaginal 0.5 estriol cream. One group received 0.5 mg. of estriol every night for two weeks, followed by twice-weekly applications of the cream for eight months, and the other group received a placebo cream in the same manner.
* p<0.005 t p<0.001 The results of the study showed a dramatic reduction in urinary tract infections in the women receiving the estriol cream compared to those receiving the placebo cream. The incidence of infection was almost 12 times greater in the placebo group (5.9 per patient year) compared to the estriol group (0.5 per patient year). According to the Israeli scientists, "The intravaginal administration of estriol prevents recurrent urinary tract infections in postmenopausal women, probably by modifying the vaginal flora." Evidence That Estriol Can Prevent Breast CancerThere is also direct evidence from animal studies and indirect evidence from human studies that estriol can prevent breast cancer. Much of this work has been done by Dr. H. M. Lemon and associates of the Department of Internal Medicine at the University of Nebraska Medical Center in Omaha. In one study, they induced mammary tumors by wholebody gamma radiation in female Sprague-Dawley rats. Subcutaneous treatment with estriol for 331-to-449 days reduced the incidence of mammary tumors from 75% in controls to 48% in the animals receiving estriol. In another study by Lemon et al., estriol was shown to have "the most significant anti-mammary carcinogenic activity of 22 tested compounds (because)...estriol is less likely to induce proliferative changes in the target organs of cancer-prone women than estrone or estradiol. " Evidence In HumansBecause of the anti-cancer effects of estriol in animals, Dr. Lemon looked at the question of whether estriol is related in any way to breast cancer in humans. He collected 24-hour urine samples from both healthy women and women with breast cancer. Dr. Lemon found that women with breast cancer had much lower levels of estriol relative to estradiol and estrone than women without breast cancer. Dr. Wright's Special Estrogen FormulaOne American doctor who has been using estriol for estrogen replacement therapy in postmenopausal women is Dr. Jonathan V. Wright of Kent, Washington, who's been prescribing estriol since the early 1980s. Dr. Wright has concluded that the best way of using estriol is in combination with the more commonly used estrogens (estradiol and estrone). His reasons for this are as follows: Dr. Wright found that, in some women, the amount of estriol required to relieve menopausal symptoms was as high as 1015 mg/day, and that as much as 12 mg/day were required to prevent osteoporosis. He found that some women suffered from nausea at such high doses of estriol that was severe enough to force him to cut down on their dosage level of the hormone. Dr. Wright determined that the ideal estrogen therapy for postmenopausal women is a combination of 80% estriol, 10% estrone, and 10% estradiol. He named his special formula Tri-estrogen and found that 2.5 mdday of tri-estrogen is usually effective in treating postmenopausal symptoms, although some women need 5 mg/day of Tri-estrogen. Another reason for including estradiol in estrogen replacement therapy is the increasing body of evidence that estrogen improves learning, memory, and other mental functions that decline with advancing age, and that estradiol may be the key estrogen in improving mental function. How To Obtain Estriol ProductsThere are several mail-order pharmacies in the United States that custom compound the estriol form of estrogen used in Europe to treat estrogen deficiency safely. Estriol can also be obtained in capsule form, or as an intravaginal cream from European companies. In pursuing estrogen replacement therapy, you should only do so under the care of a physician, preferably a gynecologist. Blood assays may not accurately reflect a women's individual need for hormone replacement. Some clinicians have told us that hot flashes, dry skin, and vaginal dryness during and after menopause may be better indicators of the need for estrogen replacement therapy than blood tests. One protocol to treat vaginal dryness is to use one gram of low potency estriol cream for seven continuous days, and then drop back to two-to-three applications a week. If low potency estriol cream does not work, you should order cream with a more potent concentration of estriol. If you take estriol in capsules, the appropriate dosage range is 4-to12 mg/day. If you wish to use Dr. Wright's formula, it is available under the name TriEst. TriEst contains:
To treat mild-to-moderate hot flashes and vaginal dryness, capsules or cream containing 1.25 mg of TriEst should be taken twice a day. For moderate to severe estrogen deficiency symptoms, 2.50 mg. of TriEst should be taken twice a day.
|
DHEA Boosts Estrogen Levels | ||||||||||||||||||||||||||||||
| DHEA replacement therapy is another natural way of replacing estrogen levels diminished by the aging process. DHEA (Dehydroepiandrosterone) is a precursor to the sex hormones. It is transformed into estrogen and testosterone within the body, all of which are needed at youthful levels to avoid the deterioration of aging. One problem with taking DHEA to replace depleted sex hormones is that the ratio of these hormones converted from DHEA is uncertain. A better way of controlling the amounts of each hormone within your body is to supplement them specifically. If you do take DHEA, it's important to understand that extra DHEA is likely to increase the levels of all your sex hormones, which may diminish your need for additional supplementation. When going on any type of hormone replacement regimen, it is vitally important for you to be tested regularly under the care of a physician in order to make whatever adjustments are necessary for optimal care. DHEA And Cancer RiskThe evidence that DHEA may prevent breast cancer is difficult to evaluate. Animal studies have shown that DHEA is very effective in preventing breast cancer, while the human studies have been inconclusive. There are studies showing that DHEA protects against human breast cancer cell proliferation by blocking estrogen receptors on breast cells, yet other studies contradict this finding. Recent studies in elderly people have found that DHEA supplementation results in overall improvement in their feeling of well being. As a result, the news media have been touting DHEA as "the first fountain of youth drug". It is interesting that DHEA produces the same anti-aging effects attributed to estrogen. It could be that some of the beneficial effects of DHEA are the result of some of the DHEA being converted into youth hormones such as estrogen and testosterone. We want to reiterate that there are contradictions in the scientific literature regarding hormone replacement therapy and cancer. Of the various hormone replacement therapies women may choose, only melatonin appears to protect against both estrogen dependent and non-estrogen dependent breast cancer. Before discussing melatonin, we'd like to point out that there are foods and nutrients you can take to augment your hormone replacement program and to help protect you against breast (and other types) of cancer. Vitamin E Protects Against Breast Cancer By Raising Estriol And Progesterone LevelsWomen with fibrocystic breast disease (mammary dysplasia) have a significantly increased risk of breast cancer. In order to test the idea that vitamin E therapy is beneficial for patients with fibrocystic breast disease, scientists at the Johns Hopkins Medical School in Baltimore conducted a double-blind trial in 17 patients and 6 controls. The patients in the study were given placebo tablets for one menstrual cycle, followed by 600 IUs a day of vitamin E (alphatocopherol acetate) for two menstrual cycles. All patients were tested for blood levels of estradiol, estriol, and progesterone. Results Of StudyThey found that 15 of 17 patients (88%) showed significant clinical improvement, confirming previous studies showing that vitamin E is an effective treatment for fibrocystic breast disease. They also found that vitamin E raised blood levels of both estriol and progesterone in fibrocystic patients, and that the ratio of both estriol and progesterone to estradiol increased as well . This may explain (in part) the therapeutic effect of vitamin E in these patients.
aMean ± S.E.
aMean ± S.E. bp<0.001 c Nine, 6 and 2 were good, fair and poor responders, respectively, as graded by published criteria.
|
Anti-Cancer Power of Coenzyme Q10 |
| Coenzyme-Q10 (ubiquinone) is a vitamin-like, non-toxic compound that plays a critical role in generating energy within the power plants of our cells (the mitochondria), and is a highly potent antioxidant that counteracts damaging free radical activity. There is a large (and rapidly growing) body of evidence that supplementation with CoQ10 can protect us against cardiovascular diseases and that CoQ10 is an effective treatment for angina (heart pain), cardiac arrhythmias, and other cardiovascular diseases. Further, CoQ10 has been shown to extend lifespan in laboratory animals. New Breast Cancer StudiesOne of the pioneering scientists in the exploration of the clinical benefits of CoQ10 is Karl Folkers of the Institute for Biomedical Research at the University of Texas in Austin. Dr. Folkers has been conducting Co Q10 research for about 35 years, and has edited several textbooks on the subject. Recently, Dr. Folkers has been collaborating with Knud Lockwood, Sven Moesgaard, and other scientists at a Private outpatient clinic in Copenhagen, Denmark to assess the benefits of CoQ10 in breast cancer patients, with some truly remarkable results. In the first study, 32 patients with breast cancer, aged 32-81, who were classified as "high-risk" because their tumors had metastasized to their lymph nodes, were given an "Adjuvant Nutritional Protocol" in addition to standard surgery and chemotherapy for 18 months. The daily nutrients added to their treatment were: 2,850 mg of vitamin-C, 2,500 mg of vitamin E, 58 mgs of beta-carotene, 387 micrograms of selenium (plus secondary vitamins and minerals), 1.2 gm of gamma linolenic acid, 3.5 grams of n-3 fatty acids, and 90 mg of CoQ10. The Danish scientists found that: "Six of the 32 paients showed partial tumor regression, none of the patients died during the study period (the expected number was four), none of the patients showed signs of further distant metastases, and the quality of life was improved (no weight loss, reduced use of pain killers) in all the patients studied. After 24 months, all the patients were still alive." Raising The Dosage of Co-Q10The positive results of this study led the scientists to increase the dose of CoQ10 to 390 mg per day in one of the patients, a 59-year-old woman with a family history of breast cancer. This woman had been operated on for removal of a malignant tumor in her left breast in July 1991. Mammography in May 1992 showed tumor tissue remaining in her left breast and other tests revealed metastasized tumor cells in her lymph nodes. The woman was started on the nutritional regimen described above in October 1991. In October 1993, her daily intake of Co Q10 was raised to 390 mg/day. "In November 1993, the tumor was no longer palpable. Mammography in December 1993 confirmed normal conditions with no signs of the tumor..." Encouraged by this complete regression of a breast tumor, they began to give 390 mg per day of CoQ10 to a 74-year old woman who had refused further surgery after learning that her breast cancer had not been eradicated by previous surgery. Late in 1993, the patient was given daily doses of 390 mg of CoQ10 and: "On January 25, 1994, clinical examination revealed no evidence of tumor or distant metastases. Mammography revealed no residual tumor. As of February 1994, therapy continues with 300 mg co Q10. Clinical condition is excellent." Additional CasesSince then, the Danish scientists (and Folkers) have reported the results of treating three additional patients with 390 mg a day of CoQ10 in addition to a conventional protocol. They reported that: "The numerous metastases in the liver of a 44-year-old patient disappeared, with no signs of metastases found elsewhere. A 49-year-old patient, on a dose of 390 mg of CoQ10, revealed no signs of tumor in the pleural cavity after six months and her condition was excellent. A 75-year-old patient with carcinoma in one breast after lumpectomy showed no cancer in the tumor bed or metastases after receiving 390 mg per day of CoQ10." Dr. Lockwood is an oncologist (in Denmark) who has been treating 200 cases of breast cancer a year for the past 35 years. He says that he has "never seen a spontaneous complete regression of a 1.5-2.0 cm. breast tumor, and has never seen a comparable regression with any conventional anti-tumor therapy." Dr. Lockwood is amazed at the remarkable anti-cancer power of Coenzyme Q10 and is continuing (with his colleagues) to treat breast cancer patients with 390 mg per day of CoQ10. Protection Against Breast Cancer With CoQ10Dr. Folkers has found that breast cancer patients have significantly lower blood levels of CoQ10 than normal people. This finding, combined with the remarkable results of treating breast cancer patients with CoQ10 in Denmark, is persuasive evidence that taking supplemental CoQ10 can protect women against breast cancer. For prevention purposes, we recommend a CoQ10 dose of 100 mg per day. Women who are at high risk for breast cancer because of a family history of the disease, or because they have already had breast cancer, should take 200-300 mg a day of CoQ10. The Benefits of Natural ProgesteroneUnlike the synthetic progestins approved by the FDA that may increase your risk of breast cancer, natural progesterone protects against many of estrogen's lethal side effects and protects against osteoporosis better than estrogen. While estrogen protects against osteoporosis by preventing the loss of bone, progesterone can actually reverse the process by increasing bone density. Dr. john Lee has found that the use of a topical progesterone cream leads to a 10% increase in bone density within 6-to-12 months, followed by an annual increase of 3%-to-5% until the bone density of his postmenopaual patients stabilizes at the levels of healthy 35-year-old women! Several prospective studies have shown a significantly higher incidence of breast cancer in progesterone-deficient women. One study, in which 1,083 women were examined, found that premenopausal women who were deficient in progesterone had a 5.4 times greater risk of breast cancer! Progesterone deficiency can also be a cause of depression, irritability, mood swings, and insomnia. If you use DHEA or other therapies to boost estrogen levels, than it is even more important for you to apply transdermal natural progesterone cream to your skin on a regular basis. Premenopausal women can use one-eighth to one quarter-teaspoon of topical natural progesterone cream every day during the 15th to 28th day of their menstrual cycle. Menopausal and postmenopausal women should use a half-teaspoon of natural progesterone cream twice daily for the first month, then reduce the amount to one-quarter of a teaspoon daily. Progesterone is absorbed through fat cells under the skin. It is, therefore, important to apply topical progesterone cream to different parts of your body every day to avoid saturating your fat cells, thereby inhibiting progesterone absorption. As with estrogen replacement therapy, it is important to have complete hormone blood tests on a regular basis to make sure you are getting enough progesterone to block estrogen's carcinogenic effects and to prevent bone loss. |
Phytochemicals Fight Breast Cancer |
| Many of the phytochemicals found in edible plants that you've been hearing so much about lately have weak estrogenic activity. These "phytoestrogens" are able to occupy the estrogen receptors on the surface of breast cells to block normal estrogen activity, thereby lowering the risk of breast cancer. Isoflavones are a large class (over 4,000) of compounds found in plants, many of which are weak estrogens. Some of the most Potent of these isoflavones are found in soybeans and soybean products such as Tofu. The isoflaivone that appears to have the most powerful anti-cancer effects is genistein, which can only be found in high concentrations in soybeans. In addition to its estrogen-blocking effects, genistein can convert malignant cancer cells back into normal cells. There have been many studies suggesting that eating soy products can help to lower the risk of breast cancer. It's been shown for example that Oriental women, who have a lower-than-normal incidence of breast cancer, consume much larger amounts of soy products than most American women. When Asianl women move to the United States, however, their intake of soy products goes down and their incidence of breast cancer goes up. When Stephen Barnes of the University of Alabama at Birmingham gave female rats large amounts of four soy products including soy protein, soy molasses, soy flour and alcohol-extracted soy protein concentrate, they found a major reduction in mammary tumor estrogen receptors, leading to a reduction in the incidence of malignant mammary tumors. In another study at the University of Alabama, supplementation with Mise Oapanese soybean paste) reduced the incidence of DMBA-induced mammary tumors in female Sprague-Dawley rats. The scientists speculated that other agents in this paste may have contributed towards its anti-cancer effect, including the antioxidants (and free radical fighters) butylated hydroxytoluene (BHT) and butylated hydroxyanisole (BHA), which are known to inhibit DMBA-induced rat mammary tumors. Phytochemicals In Cruciferous VegetablesCruciferous vegetables such as broccoli, cabbage, cauliflower, and brussels sprouts contain several compounds that produce estrogen-like activity and protect against breast cancer. In a study at the Institute For Hormone Research in New York, 12 healthy volunteers (seven men and five women) were given daily doses of 350-500 mg of one of these compounds, indole-3-carbinol (13C), which is equivalent to 10-to-12 ounces of raw cabbage or brussels sprouts. After a week, they found that the indole-3carbinol had converted estrogen into a metabolite other than the active form linked to cancer. The researchers later duplicated the same effect on estrogen of this cruciferous vegetable extract in a larger group of women. Another of these compounds -sulforaphane- found in broccoli---was found by scientists at the Johns Hopkins School Of Medicine in Baltimore to increase the synthesis of enzymes such as quinone reductase and glutathione transferase, which detoxify cancer causing chemicals within the body. High Intake Of Phytochemicals The evidence is clear that one way of helping to prevent breast cancer is to consume daily servings of fresh or steamed cruciferous vegetables, which have Potent anti-breast cancer effects. It would also be advisable to consume daily servings of other fresh vegetables such as tomatoes, lettuce, green peppers, and carrots, as well as fresh citrus Fruits, apples, melons, and other fruits--the intake of which have been shown to be associated with reduced cancer risk. An easy way of getting substantial extra intake ol vegetable extracts is to take a tablespoon of Phytofood powder every day to obtain the broccoli and cabbage concentrates that contain the most potent breast-cancer-fighting phytochemicals. Other Lifestyle FactorsThere also is evidence that the B-complex vitamins may protect against some of the toxic effects of estradiol and estrone in the body. Estrogen may produce some of its toxicity by causing vitamin B-6 deficiency. There is evidence that flax seed oil, borage oil, and fish oils may lower the production of these potentially dangerous estrogens by blocking some of their tumor initiating effects. It would also be wise to consume a low-fat diet, no more than moderate alcohol intake, and avoid environmental toxins. Studies have shown that the dangerous forms of estrogen mutants, highly toxic forms of estradiol and estrone, can be caused by a high-fat diet, excessive alcohol intake, obesity, low thyroid function, and exposure to Pesticide residues. |
Melatonin To Prevent Breast Cancer! | |
| If you take DHEA, Premarin, or any other estrogen-related drug, it is very important that you also take the pineal hormone melatonin. Melatonin blocks estrogen receptors on breast cells, stopping them from proliferating in response to estrogen and other factors that promote tumor growth. Melatonin also protects breast cell against chemical carcinogens, free radical damage, cortisol-induced damage, and non-estrogen dependent cellular changes that lead to breast cancer! Melatonin should be taken at bedtime. It usually induces drowsiness and improves the quality of sleep. Melatonin is inexpensive and readily available to Americans. Pregnant women and women seeking to become pregnant should avoid Melatonin because of its ability (in high doses) to act as a contraceptive. Until Cancer Is Cured...Use Hormone Replacement With CautionAnti-aging cell renewal hormones, precursor hormones and their metabolites include estrogen, progesterone, testosterone, DHEA, growth hormone, and insulin growth factors (ICF-1 and IGF-2).
|