Life Extension Magazine®

Ariel Soffer, MD
Q: What causes most vein symptoms?
A: Venous Reflux Disease, also known as Chronic Venous Insufficiency (CVI), affects the circulation of your blood. The main role of your veins is to return blood to the heart, but if the valves inside the veins fail, they will give way to the forces of gravity and not return blood to the heart. This backward flow is called reflux. This blood can become acidic from accumulation of metabolic waste, causing an intense inflammatory reaction resulting in symptoms such as pain and swelling.1 Venous reflux disease can lead to spider veins or thick, bulging varicose veins. Typically, varicose veins are an indicator of venous reflux, which can cause serious circulatory problems if not treated properly.
Q: What are the most common symptoms of Venous Insufficiency (VI)?
A: According to most reports, these are the five most common symptoms:2-4
- Leg pain
- Leg heaviness
- Leg throbbing
- Leg, ankle, or foot swelling
- Leg itching
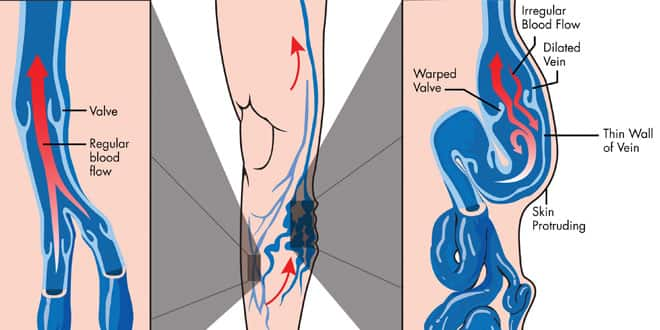
normal vein blood flow and varicose veins
In a normal vein (far left) the blood flow is only in one direction—back to the heart. When a vein becomes unhealthy blood can flow in both directions causing excess blood to pool and stretch the vein resulting in the ropey, twisted appearance of varicose veins.
Q: Can Restless Leg Syndrome be related to veins?
A: Restless Leg Syndrome causes a person to always feel the urge to move his or her legs. Restless Leg Syndrome can make it uncomfortable to do normal activities, such as sleeping through the night or traveling long distances in the car or on a plane. While there are other causes of Restless Leg Syndrome, it is a common complaint by people who have vein disease. Legs often tend to feel achy, cramped, and tired because of broken vein valves. Treatment of venous insufficiency is often very helpful in dealing with Restless Leg Syndrome.5
Q: What are “spider veins” and are they purely a cosmetic problem?

A: Spider veins are tiny, thin veins that can be seen very close to the skin’s surface caused by pooling blood. These are tiny, red, purple and/or blue veins found on the surface of the skin. They often are found in combination with slightly larger “reticular” veins, which tend to be green or blue in color. Spider veins are thought to be the result of a miniature version of the same process as varicose veins and may or may not be associated with obvious underlying varicose veins. If there is significant venous insufficiency present, which is caused by broken valves that can be identified with a simple ultrasound, any treatment is unlikely to provide lasting results. Therefore, an experienced practitioner should carefully examine a patient’s legs before attempting treatment. Spider veins, without corresponding venous insufficiency, are typically simple cosmetic issues and are relatively easily treated by experienced practitioners with injections of new mild vein irritants such as polidocanol or sotradecol.6 Laser treatment of spider veins on the face or legs can also be successful as the newer equipment is more specific to the vein and spares the surrounding tissues.6
Q: What are varicose veins?
A: Varicose veins are enlarged veins that often appear ropey and look blue or red. However, because they often occur deeper under your skin, you are not able to see them in many instances. Varicose veins are caused by unhealthy valves inside the veins.7 When these valves fail or leak, they can no longer pump blood to the heart. Gravity causes the blood to gather in the veins and makes them look enlarged, twisted or full and bulging. Aside from their unpleasant appearance, other side effects of varicose veins include pain, fatigue, itching, burning, swelling, cramping, restlessness, and throbbing, which will worsen over time if left untreated and can lead to even more serious circulatory problems.7
Q: What types of non-surgical treatments are out there for vein problems?
A: Unlike in the past, surgery is rarely necessary for vein problems anymore.7 Newer treatments, such as thermal energy (including laser or radiofrequency) or newly approved injectable sclerotherapy agents designed to painlessly destroy the damaged veins while sparing the competent ones, have become the mainstay of most phlebologists (doctors specializing in vein care).8 Additionally, certain nutraceuticals (some used frequently in Europe by prescription) have been shown in multiple studies to relieve the symptoms of varicose veins and venous insufficieny.9-16
Q: What are some of the nutraceutical treatments available for vein problems?
A: First isolated in 1925, the flavonoid diosmin is a phytonutrient that can be isolated from various plants or can be synthetically converted from the citrus flavonoid hesperidin.17 For around 40 years it has been used as an oral phlebotropic (a compound that supports the veins) compound used in the treatment of venous diseases including chronic venous insufficiency and hemorrhoids.17
In some European countries, diosmin is available only by prescription. In the United States however, it is considered a nutritional supplement.
One of the most widely used nutraceutical approaches for varicose veins is horse chestnut seed extract (Aesculus hippocastanum). Horse chestnut seed extract is widely used in Europe for chronic venous insufficiency.
Horse chestnut seed extract has demonstrated impressive efficacy in relieving the symptoms of chronic venous insufficiency, effectively reducing leg volume, alleviating leg pain, improving edema, and averting itching.18 Horse chestnut has been reported to increase blood circulation by inhibiting the breakdown of vein walls and improving venous contractility.18,19
The active ingredient in horse chestnut seeds is a chemical called escin.18 Studies suggest that twice-daily horse chestnut extract, containing 50 mg escin, is as effective as standard therapy with compression stockings in the early stages of chronic venous insufficiency.20,21 (The corresponding dose of horse chestnut extract is 250 mg taken twice daily, standardized at 20% [50 mg] escin.)
Q: What do the new lasers and injectables do for vein problems?
A: Endovenous Laser Treatment. Endovenous Laser Treat-ment (EVL) is a technology used to treat varicose veins, which involves heating the inside of the vein, causing it to seal shut and disappear.22 During Endovenous Laser Treatment, a very thin laser fiber is inserted into the damaged vein. It is largely painless and can be performed on an outpatient basis, allowing patients to go back to work the very same day. In capable, experienced hands, this technology has been extremely successful and has largely eliminated the need for the more invasive vein-stripping surgery.22 To ensure satisfactory long-term results, most Endovenous Laser Treatment patients will require some sclerotherapy in conjunction with Endovenous Laser Treatment to treat their varicose and smaller veins. The result is often a complete resolution of symptoms and a vast improvement in aesthetic appearance.
Sclerotherapy. Sclerotherapy is an injection treatment used to eliminate small to medium size varicose veins and spider veins.23 Sclerotherapy is affordable, does not require anesthetic, and there is no downtime associated with this simple procedure. Sclerotherapy utilizes a very fine needle to inject a solution, known as a sclerosant, into the varicose or “spider vein.”23 Most patients compare the discomfort of the needle to an ant bite. The location of the vein determines if this procedure is done with or without ultrasound guidance. Different solutions are used, depending on the type of the vein, and different strengths of the solutions are used, based on the size of the vessel. Once injected, the cells that line the vein wall (endothelium) will become irritated, inflamed, and damaged.23 External pressure is applied using cotton balls, tape, and support hose. The compression causes the vein walls to seal together, sealing the vein off from the rest of the vein network in your leg, and the vein can no longer transport blood. Your body will then break down and absorb the damaged vein, and naturally redirect the blood flow to healthy veins. Upon the completion of healing, the vein is no longer visible. It should be noted that the same vein may have to be treated more than once during your sclerotherapy sessions. The process is very similar to how your body heals a bad bruise. Spider veins do not have any known useful function and eliminating them will not affect your circulation. Reducing or eliminating varicose veins can improve your circulation and symptoms of heaviness, aching, and fatigue.

Ultrasound-guided Sclerotherapy. Ultrasound-guided Sclerotherapy is used for larger and deeper varicose veins that cannot be treated with the laser for varying reasons, including their visibility, location, and/or morphology.24 The ultrasound offers your physician the ability to precisely target the exact location to optimize treatment results.25 Ultrasound guided sclerotherapy is similar to traditional sclerotherapy. The only difference is that the doctor uses ultrasound technology to see the veins beneath the skin. Using the ultrasound image as a guide, the doctor can place sclerosing foam directly into the abnormal vein, thereby redirecting blood flow to healthy veins.24,25 The treated vein closes and, over weeks or months, becomes an imperceptible thread beneath the skin.
Conservative Treatment. The objective of the conservative approach in treating varicose veins is to help support the venous circulation of the legs in order to slow the development of new veins and to minimize symptoms. These treatment methods will not cure or eliminate existing vein problems; however, they will help slow the progression of the disease and alleviate symptoms such as swelling, aching, and cramping. As a result, conservative treatment is most suitable for people who are sick, elderly, or pregnant. Some of the more popular conservative treatments are:9-16,26
- Support compression stockings provide external graduated counter-pressure to aid in venous blood flow to the heart. They reduce pooling and pressure in the veins and may also reduce the risk of forming a deep vein blood clot. Consider wearing them during long plane or car rides.
- Making lifestyle changes, including losing weight and increasing activity and exercise.
- Preventative measures. There is no known scientific method for preventing varicose veins, but there are ways of improving your circulation and muscle tone, thereby reducing the risk of developing varicose veins or getting additional ones. Some of the more popular preventive measures are:
— Elevating your legs. Elevate your legs when possible by keeping your feet positioned higher than your heart level to reduce pooling and pressure on your legs.
— Exercising daily. Walking, climbing stairs, cycling, and swimming keep your calf muscles in motion to activate the calf muscle pump. This reduces pooling and pressure in the veins.
— Maintaining a healthy body weight. Maintaining your ideal body weight will reduce excess pressure on your legs.
— Actively moving. On long car or plane trips, activate your calf muscle pump by flexing your ankles periodically to pump the blood out of your legs (simulating walking). During periods of prolonged sitting or standing, flex your ankles 10 times and repeat this every 10 minutes. You should also consider stopping for short walks every few hours.
— Avoiding sitting extensively. Try to avoid sitting for extended periods throughout your day.
— Avoiding excessive heat. Try to avoid excess heat on your legs, such as hot tubs and hot baths. Heat tends to increase vein distention and lead to more pooling of blood.
— Nutraceutical treatment: As explained in greater detail above.
While there are a number of different treatment options available for varicose and spider veins, in our experience, we have found that a treatment consisting of a combination of the treatments above has proven to be most effective in the treatment of varicose and spider veins and related symptoms. Our refined use of sclerotherapy, combined with thermal laser treatments, allows us to uniquely address the needs of our patients by treating the smallest spider vein to the largest ropelike varicose vein. The great news is that none of the treatments requires hospitalization or surgery. All procedures are done in our office and patients can be back on their feet doing their normal routine that very same day.
Q: How do you measure progression of your treatment?

A: Clinical photography is one of the most important tools a phlebologist may use to easily illustrate the progress of treatment to the patient. Because every patient responds to treatments at different rates, clinical photography also assists practitioners in adjusting their treatment strategy. Additionally, since improvement is gradual over time in certain instances, the use of clinical photography is a wonderful tool for practitioners to better manage their patients’ expectations by easily showing the progress of their veins when compared to a baseline. Most experienced practitioners utilize clinical photography in some form, and recent improvements in digital equipment technology make it easily accessible to the patient.
Dr. Soffer is a Board Certified Cardiovascular Specialist, Member of the American College of Phlebology and Fellow of the American College of Cardiology. He is also the Medical Expert for ABC News-Miami and where he has the weekly segment “Dr. Soffer’s Second Opinion” on 5pm ABC-Miami News. The Soffer Health has Private Offices in Dade and Broward County www.sofferhealth.com
If you have any questions on the scientific content of this article, please call a Life Extension® Health Advisor at 1-866-864-3027.
References
- McDonagh PF. The microvascular pathophysiology of chronic venous insufficiency. Yale J Biol Med. 1993 Jan-Feb; 66(1): 27–36.
- Available at: http://health.nytimes.com/health/guides/disease/venous-insufficiency/overview.html. Accessed February 14, 2013.
- Available at: http://www.ucdmc.ucdavis.edu/vascular/diseases/cvi.html. Accessed February 14, 2013.
- Partsch H. Varicose veins and chronic venous insufficiency. Vasa. 2009 Nov;38(4):293-301.
- Hayes CA, Kingsley JR, Hamby KR, Carlow J. The effect of endovenous laser ablation on restless legs syndrome. Phlebology. 2008;23(3):112-7.
- Moreno-Moraga J, Hernández E, Royo J, et al. Optimal and safe treatment of spider leg veins measuring less than 1.5 mm on skin type IV patients, using repeated low-fluence Nd:YAG laser pulses after polidocanol injection. Lasers Med Sci. 2012 Aug 11. [Epub ahead of print]
- Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/pmh0002099. Accessed February 14, 2013.
- Available at: http://www.nlm.nih.gov/medlineplus/ency/article/007395.htm. Accessed February 14, 2013.
- Cappelli R, Nicora M, Di Perri T. Use of extract of Ruscus aculeatus in venous disease in the lower limbs. Drugs Exp Clin Res. 1988;14(4):277-83.
- Vanscheidt W, Jost V, Wolna P, et al. Efficacy and safety of a Butcher’s broom preparation (Ruscus aculeatus L. extract) compared to placebo in patients suffering from chronic venous insufficiency. Arzneimittelforschung. 2002;52(4):243-50.
- Aesculus hippocastanum (Horse chestnut). Monograph. Altern Med Rev. 2009 Sep;14(3):278-83.
- Suter A, Bommer S, Rechner J. Treatment of patients with venous insufficiency with fresh plant horse chestnut seed extract: a review of 5 clinical studies. Adv Ther. 2006 Jan-Feb;23(1):179-90.
- Maksimović ZV, Maksimović M, Jadranin D, Kuzmanović I, Andonović O. Medicamentous treatment of chronic venous insufficiency using semisynthetic diosmin--a prospective study. Acta Chir Iugosl. 2008;55(4):53-9.
- Lyseng-Williamson KA, Perry CM. Micronised purified flavonoid fraction: a review of its use in chronic venous insufficiency, venous ulcers and haemorrhoids. Drugs. 2003;63(1):71-100.
- Cesarone MR, Belcaro G, Rohdewald P, et al. Comparison of Pycnogenol and Daflon in treating chronic venous insufficiency: a prospective, controlled study. Clin Appl Thromb Hemost. 2006 Apr;12(2):205-12.
- Cesarone MR, Belcaro G, Rohdewald P, et al. Improvement of signs and symptoms of chronic venous insufficiency and microangiopathy with Pycnogenol: a prospective, controlled study. Phytomedicine. 2010 Sep;17(11):835-9.
- Available at: http://www.thorne.com/altmedrev/.fulltext/9/3/308.pdf. Accessed February 15, 2013.
- Available at: http://www.thorne.com/altmedrev/.fulltext/14/3/278.pdf. Accessed February 15, 2013.
- Available at: http://acudoc.com/cardiovascular.pdf. Accessed February 15, 2013.
- Ottillinger B, Greeske K. Rational therapy of chronic venous insufficiency--chances and limits of the therapeutic use of horse-chestnut seeds extract. BMC Cardiovasc Disord. 2001;1:5. Epub 2001 Dec 7.
- Diehm C, Trampisch HJ, Lange S, Schmidt C. Comparison of leg compression stocking and oral horse-chestnut seed extract therapy in patients with chronic venous insufficiency. Lancet. 1996 Feb 3;347(8997):292-4.
- Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of saphenous vein reflux: long-term results. J Vasc Interv Radiol. 2003 Aug;14(8):991-6.
- Khunger N, Sacchidanand S. Standard guidelines for care: sclerotherapy in dermatology. Indian J Dermatol Venereol Leprol. 2011 Mar-Apr;77(2):222-31.
- Liu X, Jia X, Guo W, et al. Ultrasound-guided foam sclerotherapy of the great saphenous vein with sapheno-femoral ligation compared to standard stripping: a prospective clinical study. Int Angiol. 2011 Aug;30(4):321-6.
- Kanter A, Thibault P. Saphenofemoral incompetence treated by ultrasound-guided sclerotherapy. Dermatol Surg. 1996 Jul;22(7):648-52.
- Available at: http://www.womenshealth.gov/publications/our-publications/fact-sheet/
varicose-spider-veins.cfm#K. Accessed February 15, 2013.

