Life Extension Magazine®

In 1938, Orson Welles’ fictional broadcast of Earth being invaded by Martians was aired on CBS Radio. The resulting hysteria drove over a million Americans to flee into hiding or force open armories so citizens could defend against the attacking space monsters.
CBS’s on-air dramatization of the H.G. Wells novel “War of the Worlds” is history’s most effective manipulation (by a single broadcast) of the perception of reality in the consciousness of the masses.
This kind of chaos is not confined to last century. In September 2012, the American Medical Association published a study by three Greek doctors that proclaimed there is no value to recommending omega-3 supplements to cardiac patients.1
Consumers were misled as the media inaccurately represented the study’s findings. This manipulation of reality will cause millions of needless deaths throughout the world if not retracted.
I titled this piece “Science by Ambush” because the media turned this flawed report into headline news and, in the process, failed to include an objective rebuttal.
This article will expose flaws that discredit this study’s conclusions, the media’s inappropriate portrayal of this study, the public’s lack of knowledge about how to use omega-3s, and the inability of most people to understand that the successful treatment of atherosclerotic disease requires more than one intervention.American Medical Association Attack on Fish Oil

The September 12, 2012, issue of the Journal of the American Medical Association published a data analysis of 20 self-selected prior studies on fish oil and vascular disease.
Their findings showed that in response to a modest daily intake of fish oil (only 1,370 milligrams of EPA/DHA), the following positive effects were observed: 1
- 9% reduction in cardiac death
- 13% reduction in sudden death
- 11% reduction in myocardial infarction (heart attack)
- 4% reduction in all-cause mortality
The authors of this study claimed that the data they assembled did not have “statistically significant association” and therefore no likely benefits were observed in the 20 studies they reviewed where a modest dose of fish oil was used for a short treatment term (median 2 years).
Not all participants in this analysis took fish oil capsules. Some of the estimated daily EPA/DHA intake was based on food guidance counseling. Omitted from the authors’ analysis were studies showing more robust heart attack reduction in response to higher doses of fish oil used by enlightened consumers today.
The authors nonetheless concluded that their observations “do not justify the use of omega-3 as a structured intervention in everyday clinical practice or guidelines supporting dietary omega-3 administration.”1
The Raging Inferno
If you had to rely on the media’s sensationalist reporting of the study published in the Journal of the American Medical Association (JAMA), you might think there is no value to omega-3 supplementation.
Yet the JAMA study itself reported on published benefits of fish oil as follows: 1
- Substantial reduction in triglycerides (even the FDA recognizes this benefit).
- Reduction in serious arrhythmias (irregular heartbeat).
- Decreased platelet aggregation (protects against clots forming in arteries).
- Modest reduction in blood pressure.
There are other ways that fish oil helps prevent heart attack, such as protecting against inflammation, but just the four benefits outlined in the JAMA study itself provide a scientific rationale for anyone concerned about vascular health to ensure adequate omega-3 intake.
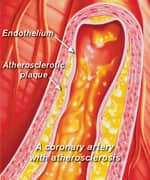
What most physicians do not understand, however, is the magnitude of damage that is already present in the inner arterial lining of cardiac patients. These patients already suffered a heart attack or developed problems that required intervention with stents, bypass surgery, and/or aggressive drug therapy, and thus had significant pre-existing arterial disease.
In my previous career, I was involved in thousands of autopsy cases where I could see and feel the effects of aging in the form of blocked and hardened arteries throughout a deceased person’s body. There was often such severe arterial occlusion that my colleagues would question how the person lived as long as they did.
Arterial disease begins at birth and progresses as we mature. Over a certain age, many people become victims of “accelerated atherosclerosis” whereby a coronary artery that was only 30% occluded three years earlier rapidly becomes 90–100% blocked.
What is remarkable is how much damage can be inflicted to our vital circulatory system before death ensues. The point I’m getting at is that by the time people manifest outward signs of vascular disease (such as needing a coronary stent), there is a raging inferno going on inside their arterial walls that is not going to be extinguished with fish oil alone.
Most of the subjects in these studies analyzed by JAMA had already suffered a heart attack or coronary artery blockage and the fish oil was being used for “secondary prevention” purposes. At this advanced stage, the window had long ago closed for a modest dose of any treatment to be effective.
To clarify, let’s say you are barbecuing outdoors and you accidentally ignite a bush next to your house. You turn your garden hose on full blast and rapidly extinguish the fire. Based on your experience, you can categorically state that garden hoses are effective in preventing houses from burning down.
Now let’s say you come home and find your house engulfed in flames. You take your garden hose and turn it only half-way on, but your house burns to the ground anyway. At that point you state that garden hoses are useless in preventing houses from being destroyed by fire.
While there is solid evidence to document that fish oil is more effective than a garden hose in this analogy, what JAMA has in essence published are selected efforts of mainstream doctors using an inadequate dose of fish oil, over too short a time period, to put out a raging inferno going on inside the arteries of cardiac patients.
Comparison With Statin Drugs
By reducing LDL cholesterol, statin drugs have been shown to lower heart attack risk.2
A healthy person without arterial disease can sometimes get by with using a modest dose (10 mg/day) of a drug like simvastatin. Along with healthier dietary patterns, this can slash LDL levels from a dangerous 140 mg/dL to the safe range for healthy people now recognized to be under 100 mg/dL.
This dose of statin drug, however, will not reduce LDL-C levels aggressively enough for those with pre-existing arterial disease. These individuals need to get their LDL under 70 mg/dL, which, in the example cited, may require a daily dose of simvastatin of 80 mg per day. It is at these high doses that statin drugs inflict most of their nasty side effects.
Since the medical establishment recommends that those with pre-existing arterial disease take higher doses of statin drugs, it is ludicrous to think that a modest dose of fish oil would show a significant effect on the relatively unhealthy patient populations analyzed in the JAMA report.How Much EPA/DHA Should Be Consumed Each Day?

About 60% of your brain mass consists of fats that comprise vital cell membranes.3 DHA is the dominant omega-3 fat in healthy brain cells. Since people cannot make DHA internally, it has to come from diet or supplemental sources.
For the JAMA authors to state that there is no place in clinical practice to encourage omega-3 intake borders on medical negligence. The fact that they hand-selected studies where inadequate doses of omega-3s were used hints at a sizeable bias against non-drug approaches to treating disease.
Based on the totality of evidence showing multiple health benefits associated with greater omega-3 intake, Life Extension® long ago recommended that members should supplement with 2,400 mg of EPA/DHA each day. This recommendation was based on the three assumptions listed on the next page.
- Foundation members are health-conscious individuals who consume food sources of omega-3s like cold-water fish, thus providing greater average intake of omega-3 than 2,400 mg daily.
- Foundation members take annual blood tests that measure triglyceride levels. If triglycerides are over 100 mg/dL of blood, there would be a greater consumption of omega-3s, along with lifestyle, drug, and other supplement alterations. (Some people, for instance, require daily doses of 4,800 mg of EPA/DHA to suppress artery-clogging triglycerides.)
- Findings from Omega Score blood test results show that at least 2,400 mg a day of EPA/DHA is needed to achieve optimal omega-3 blood levels. (Some people require more than 2,400 mg of omega-3s to boost blood levels.)
The media used the JAMA study to create headlines like “Fish oil supplements don’t prevent heart attacks, study says.”4 The JAMA report, however, was based on an average daily intake of only 1,370 mg of EPA/DHA in individuals who mostly suffered significant pre-existing arterial disease, i.e., atherosclerosis. In fact, half of the studies included in the meta-analysis used an omega-3 dose of less than 1,000 mg daily. This amount of EPA/DHA is too low to reverse the underlying progression of atherosclerosis that most of the study group suffered.
The unhealthy study subjects used in the JAMA study consisted of population groups in countries throughout the world. Based on what the JAMA authors wrote, these study subjects presumably consumed less than 58% of the minimum amount of EPA/DHA that Life Extension members take. Some of these population groups took no other supplement to protect against heart attack since these nutrients are not openly sold in those countries.
I use the term “presumably consumed” in the previous paragraph because it is not clear that study subjects even got 58% of the EPA/DHA they needed. The JAMA study results were based either on patients instructed to take fish oil capsules or patients provided with “dietary guidance counseling.” This kind of diet counseling is notoriously unreliable, especially over the longer term when people tend to gravitate back to unhealthy dietary habits. The same is often true of people who are told to swallow large fish oil capsules by their doctors but fail to comply for all kinds of reasons including the fact that they don’t like swallowing large capsules!
As you will read in the sidebar on page 13, the findings from the JAMA study (where lower-dose EPA/DHA was inconsistently used on unhealthy patient groups for a relative short term) have nothing to do with what health-conscious people are doing today to guard against heart attack, which includes taking the proper dose of EPA/DHA each day.
Why Most Consumers Don’t Benefit From Fish Oil

The environment that we at Life Extension exist in is far removed from the mainstream. We are privileged to interact with exceptional physician/scientists and the world’s most knowledgeable health consumers (i.e., our members).
Recently, we found ourselves so out of touch with the mainstream that we went to considerable expense to empanel outside focus groups to educate us on how the lay public thinks about nutrition and their health. To participate in these focus groups, people had to be health-conscious consumers who used dietary supplements. The level of ignorance uncovered by these focus group sessions was appalling.
Virtually all the focus group participants had “heard” good things about omega-3s, but they had no idea how much they were taking or how much EPA/DHA they should use. Most of them claimed to purchase omega-3 supplements on a somewhat irregular basis, usually when they saw them displayed on a pharmacy or supermarket shelf. Some claimed to take one fish oil capsule daily while others claimed to take them when they would remember.
If a survey were conducted to identify people who took omega-3 supplements, virtually every participant in these focus groups would have been categorized as an omega-3 supplement user. Yet virtually none of them were taking the potency needed to stave off heart disease.
When conventional doctors and the media claim that people don’t benefit from supplements, they are often correct in that most consumers have no idea how much of what supplement they should take to stave off disease. This should not dissuade knowledgeable individuals, who know what to take and have the discipline to do so on a consistent basis, from following an evidence-based program that includes at least 2,400 mg of supplemental EPA/DHA daily along with healthy dietary patterns.
Methodology Problems with the JAMA Meta-Analysis

Flaws in the design of the JAMA meta-analysis of 20 self-selected studies call its findings into question for the following reasons:
Inclusion of trials of poor methodological quality. Nearly half of the sample size of the meta-analysis came from two open-label trials. Open-label trials allow both the subjects and researchers to know what treatment is being provided in the study. This type of study is considered to be of inferior quality compared to double-blind, placebo-controlled trials, where researchers and subjects do not know which intervention the subjects are receiving.
High level of variability in the trials’ cardiovascular event rates & baseline risk. There was a high degree of variability in the baseline cardiovascular risk and cardiovascular event rates in the trials included in this meta-analysis. This means it was difficult to assess which subjects were at greater risk of heart attack at baseline. If those given fish oil, for instance, also had higher vascular risk at the beginning of the study, then the validity of the data is severely compromised.
Limited number of studies included. Only 20 of 3,635 studies the authors examined were used in this meta-analysis. This provides a very limited view of the research that has been conducted on fish oil for cardiovascular disease.
There has been a significant amount of research conducted on the cardiovascular benefits of fish oil beyond what was selected for the JAMA analysis. For example, in a PubMed.gov (U.S. National Library of Medicine) search for clinical trials of “fish oil and triglycerides,” there were over 500 results.
Good Ratings for the Media
Just imagine being in the “news” business where every day you have to generate attention-grabbing headlines to sell newspapers or attract viewers.
You see a study published in the Journal of the American Medical Association meant for doctors, but since it relates to a popular dietary supplement, you have a sound-bite headline for the day. No need to look at details — such as the JAMA study stating that even subjects who consumed inadequate doses of fish oil appeared to derive some reductions in heart attack risk.
Just hype up the JAMA study’s conclusion and you have yourself a startling headline that most of your audience will want to know more about, i.e. ambush journalism.
This is how the general public makes their life-and-death decisions, which is rather pathetic considering we live in a world where most everyone has Internet access to assess the facts for themselves.
Bottom Line: The subjects in the JAMA report were people with existing heart problems, the dosages they were taking were too small, and they probably were not taking the additional supplements that have long been recommended to generate a multi-pronged attack against heart disease.
What Do Humans Need To Do To Prevent Atherosclerosis?
The aging process damages blood vessels even when conventional risk factors such as cholesterol and blood pressure are within normal ranges.
Despite aggressive intervention with diet, exercise, supplements, and drugs, pathological changes still occur in the arterial wall that predispose aging adults to vascular diseases. The encouraging news is that validated methods have been developed to address the underlying reason why arteries become occluded as people reach the later stages of their lives.
For the past 40 years, the standard way to treat coronary atherosclerosis has been to bypass the blocked arteries. Recuperation from coronary bypass surgery can take months, and some patients are afflicted with lifetime impairments such as memory loss, chronic inflammation, and depression. Coronary artery stenting has become more common in recent years, but this is not a cure for systemic atherosclerosis.
The scientific literature reveals that atherosclerosis is associated with high blood levels of C-reactive protein,18-26 insulin,27-32 iron,33-36 LDL,37-42 homocysteine,25,26,43-46 fibrinogen,25,47-50 and triglycerides,51-53 along with low levels of HDL54-56 and testosterone57-62 (in men). Optimizing blood levels of these substances can dramatically reduce heart attack and stroke risk.Cardiologists Only Partially Correct Atherogenic Risk Factors
Prescribing a statin drug is what doctors typically do to prevent and treat coronary atherosclerosis. Cholesterol and LDL, however, are only two players in the atherosclerosis process.
There are now two fish oil “drugs” approved by the FDA to lower triglycerides. Fish oil also protects against atherosclerosis by reducing inflammation63-71 and inhibiting abnormal platelet aggregation.72-76 But even fish oil and statin drugs are not going to adequately counteract all factors involved in coronary artery disease.
Mainstream cardiologists fail to appreciate that coronary atherosclerosis is a sign of systemic arterial dysfunction requiring aggressive therapy to correct.
To read more about the steps you need to take to reduce your odds of being stricken with a vascular disorder, refer to the articles on pages 68 and 78 of this month’s issue.
How We Protect You
Life Extension’s annual Blood Test Super Sale commences April 1, 2013. The reason I am alerting you early is to enable you to start preparing for your annual comprehensive blood tests.
Make sure, for example, that you take your omega-3 and vitamin D supplements with the heaviest meal of the day. These fat-soluble nutrients absorb far better when consumed with the meal of the day that contains the most fat. A problem we fear occurs in clinical studies is that participants take fat-soluble nutrients on relatively empty stomachs, which leads to poor absorption and subsequent failure to derive benefits.
The extensive focus group sessions we conducted reveal the typical consumer has no idea what they need to do to protect against the degenerative diseases of aging.
We provide our members with every means of support possible, from access to knowledgeable health advisors and low-cost comprehensive blood testing, to accurately reported scientific data and ongoing clinical research.
The public, on the other hand, is left to rely on a sound-bite frenzied news media for health data, which often involves flouting a scary medical headline without assessing a story’s veracity. I call this science by ambush because it blind sides an established principle, and denies an opportunity for meaningful rebuttal!
For longer life,
William Faloon
Higher-Dose Fish Oil Provides Heart Benefits

A number of studies have indicated that higher doses of fish oil leads to beneficial effects in preventing cardiovascular disease events or reducing risk factors. For example:
A randomized, placebo-controlled trial found 1,800 mg of combined EPA plus DHA was associated with a 10% lower rate of cardiac events, 12% lower rate of non-fatal infarctions, and an almost 11% lower rate of cardiac deaths.5
In a large intervention study, 18,000 patients were randomized to receive either a statin medication alone or a statin plus 1,800 mg of EPA-fish oil daily. After 5 years, those with a history of coronary artery disease had a 19% lower rate of major coronary events in the statin-plus EPA-fish oil group compared to the statin-only group.6
A randomized, double-blind, placebo-controlled trial with chronic hemodialysis patients found that 1,700 mg of omega-3 fatty acids daily was associated with a 70% reduction in the relative risk of myocardial infarction.7
A randomized, controlled trial using 3,300 mg of EPA and DHA (and then a decreased dosage) found a trend toward lower cardiovascular event occurrence with fish oil supplementation. Seven cardiovascular events occurred in the placebo group (not given fish oil) while only two cardiovascular events occurred in the fish oil-supplemented group during the study.8
A meta-analysis with an average fish oil dose of 3,700 mg found lowered systolic blood pressure by an average 2.1 mmHg and diastolic by 1.6 mmHg.9
In a randomized trial with peripheral arterial disease patients, 2,000 mg of omega-3 fatty acids daily resulted in a 49% improvement in flow-mediated dilation, a marker of endothelial cell health.10
In contrast to the findings of the JAMA meta-analysis, two important studies demonstrated significant benefits with even moderate fish oil doses:
The GISSI-Prevenzione study (a large, randomized, controlled trial) found that 1,000 mg/day of EPA and DHA in 11,323 patients with a history of recent myocardial infarction reduced the risk of total mortality by 20% and sudden death by 45%.11,12
The DART study — a randomized, controlled trial that examined the effects of advising 2,033 subjects to increase dietary fatty fish — revealed a 29% reduction in all-cause mortality compared with those not advised.13
The Journal of the American Medical Association (JAMA) meta-analysis also conflicts with other reviews of fish-oil research. Other meta-analyses have demonstrated a reduced risk of cardiovascular disease outcomes in those supplemented with omega-3 fatty acids from fish oil. For example:
A 2009 meta-analysis of randomized, controlled trials found that dietary supplementation with omega-3 fatty acids reduced the incidence of sudden cardiac death in subjects with prior myocardial infarction.14
Another 2009 meta-analysis of randomized, controlled trials found that dietary supplementation with omega-3 fatty acids reduced the risk of cardiovascular death, sudden cardiac death, all-cause mortality, and non-fatal cardiovascular events in patients with a history of certain cardiovascular events or risk factors.15
A 2008 meta-analysis found a significant reduction in death from cardiac causes with fish oil supplementation.16
A 2002 meta-analysis of randomized, controlled trials concluded that omega-3 fatty acids reduced overall mortality, mortality due to myocardial infarction, and sudden death in patients with coronary heart disease.17
References
- Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS. Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis. JAMA. 2012 Sep 12;308(10):1024-33.
- Available at: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/heart-disease-risk-reduction. Accessed January 15, 2013.
- Chang CY, Ke DS, Chen JY. Essential fatty acids and human brain. Acta Neurol Taiwan. 2009 Dec;18(4):231-41.
- Available at: http://www.usatoday.com/news/health/story/2012-09-11/heart-omega-3/57750182/1. Accessed December 3, 2012.
- Singh RB, Niaz MA, Sharma JP, et al. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival. Cardiovasc Drugs Ther. 1997;11(3):485-91.
- Yokoyama M, Origasa H, Matsuzawa M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369(9567):1090-8.
- Svensson M, Schmidt EB, Jørgensen KA, et al. N-3 fatty acids as secondary prevention against cardiovascular events in patients who undergo chronic hemodialysis: a randomized, placebo-controlled intervention trial. Clin J Am Soc Nephrol. 2006 Jul;1(4):780-6.
- von Schacky C, Angerer P, Kothny W, et al. The effect of dietary omega-3 fatty acids on coronary atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1999;130(7):554-62.
- Geleijnse JM, Giltay EJ, Grobbee DE, et al. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20(8):1493-9.
- Schiano V, Laurenzano E, Brevetti G, et al. Omega-3 polyunsaturated fatty acid in peripheral arterial disease: effect on lipid pattern, disease severity, inflammation profile, and endothelial function. Clin Nutr. 2008 Apr;27(2):241-7.
- Marchioli R, Barzi F, Bomba E, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-Prevenzione. Circulation. 2002 Apr 23;105(16):1897-903.
- Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc2909229. Accessed January 15, 2013.
- Burr ML, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989 Sep 30;2(8666):757-61.
- Zhao YT, Chen Q, Sun YX, et al. Prevention of sudden cardiac death with omega-3 fatty acids in patients with coronary artery disease: a meta-analysis of randomized controlled trials. Ann Med. 2009;41(4):301-10.
- Marik PE and Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clin Cardiol. 2009;32(7):365-72.
- León H, Shibata MC, Sivakumaran S, et al. Effect of fish oil on arrhythmias and mortality: systematic review. BMJ. 2008;337:a2931.
- Bucher HC, Hengstler P, Schindler C, et al. N-3 polyunsaturated fatty acids in coronary heart disease: a meta-analysis of randomized controlled trials. Am J Med. 2002;112(4):298-304.
- Piechota W, Piechota W. Correlation of high-sensitivity CRP concentration with the extent of coronary atherosclerosis in men with symptoms of ischemic heart disease. Pol Merkur Lekarski. 2005 May;18(107):511-5.
- Choi EY, Yan RT, Fernandes VR, et al. High-sensitivity C-reactive protein as an independent predictor of progressive myocardial functional deterioration: the multiethnic study of atherosclerosis. Am Heart J. 2012 Aug;164(2):251-8.
- Van Der Meer IM, De Maat MP, Hak AE, et al. C-reactive protein predicts progression of atherosclerosis measured at various sites in the arterial tree: the Rotterdam Study. Stroke. 2002 Dec;33(12):2750-5.
- Masood A, Jafar SS, Akram Z. Serum high sensitivity C-reactive protein levels and the severity of coronary atherosclerosis assessed by angiographic gensini score. J Pak Med Assoc. 2011 Apr;61(4):325-7.
- Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of C- reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998 Aug 25;98(8):731-3.
- Auer J, Berent R, Lassnig E, Eber B. C-reactive protein and coronary artery disease. Jpn Heart J. 2002 Nov;43(6): 607-19.
- Agmon Y, Khandheria BK, Meissner I, et al. C-reactive protein and atherosclerosis of the thoracic aorta: a population-based transesophageal echocardiographic study. Arch Intern Med. 2004 Sep 13;164(16):1781-7.
- Ridker PM, Stampfer MJ, Rifai N. Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA. 2001 May 16;285(19):2481-5.
- Jarosz A, Nowicka G. C-reactive protein and homocysteine as risk factors of atherosclerosis. Przegl Lek. 2008 65(6): 268-72.
- Bonora E, Kiechl S, Willeit J, et al. Insulin resistance as estimated by homeostasis model assessment predicts incident symptomatic cardiovascular disease in caucasian subjects from the general population: the Bruneck study. Diabetes Care. 2007 Feb;30(2):318-24.
- Sundell J, Luotolahti M. Association between insulin resistance and reduced coronary vasoreactivity in healthy subjects. Can J Cardiol. 2004 May 15;20(7):691-5.
- Stochmal E, Szurkowska M, Czarnecka D, et al. Association of coronary atherosclerosis with insulin resistance in patients with impaired glucose tolerance. Acta Cardiol. 2005 Jun;60(3):325-31.
- Takahashi F, Hasebe N, Kawashima E, et al. Hyperinsulinemia is an independent predictor for complex atherosclerotic lesion of thoracic aorta in non-diabetic patients. Atherosclerosis. 2006 Aug;187(2):336-42.
- Stout RW. The relationship of abnormal circulating insulin levels to atherosclerosis. Atherosclerosis. 1977 May;27(1):1-13.
- Chien KL, Lee YT, Sung FC, Hsu HC, Su TC, Lin RS. Hyperinsulinemia and related atherosclerotic risk factors in the population at cardiovascular risk: a community-based study. Clin Chem. 1999 Jun;45(6 Pt 1):838-46.
- Howes PS, Zacharski LR, Sullivan J, Chow B. Role of stored iron in atherosclerosis. J Vasc Nurs. 2000 Dec;18(4):109-14; quiz 115-6.
- Chau LY. Iron and atherosclerosis. Proc Natl Sci Counc Repub China B. 2000 Oct;24(4):151-5.
- Kraml P, Potockova J, Koprivova H, et al. Ferritin, oxidative stress and coronary atherosclerosis. Vnitr Lek. 2004 Mar;50(3):197-202.
- Minqin R, Watt F, Huat BT, Halliwell B. Correlation of iron and zinc levels with lesion depth in newly formed atherosclerotic lesions. Free Radic Biol Med. 2003 Mar 15;34(6):746-52.
- Montalcini T, Gorgone G, Federico D, et al. Association of LDL cholesterol with carotid atherosclerosis in menopausal women affected by the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2005 Oct;15(5):368-72.
- Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004 Mar 3;291(9):1071-80.
- Reed DM, Strong JP, Resch J, Hayashi T. Serum lipids and lipoproteins as predictors of atherosclerosis. An autopsy study. Arteriosclerosis. 1989 Jul-Aug;9(4):560-4.
- Cromwell WC, Otvos JD. Low-density lipoprotein particle number and risk for cardiovascular disease. Curr Atheroscler Rep. 2004 Sep;6(5):381-7.
- Teo KK, Burton JR, Buller C, Plante S, Yokoyama S, Montague TJ. Rationale and design features of a clinical trial examining the effects of cholesterol lowering and angiotensin-converting enzyme inhibition on coronary atherosclerosis: Simvastatin/Enalapril Coronary Atherosclerosis Trial (SCAT). Can J Cardiol. 1997 Jun;13(6):591.
- Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002 Nov 14;347(20):1557-65.
- Rasouli ML, Nasir K, Blumenthal RS, Park R, Aziz DC, Budoff MJ. Plasma homocysteine predicts progression of atherosclerosis. Atherosclerosis. 2005 Jul;181(1):159-65.
- Montalescot G, Ankri A, Chadefaux-Vekemans B, et al. Plasma homocysteine and the extent of atherosclerosis in patients with coronary artery disease. Int J Cardiol. 1997 Aug 8;60(3):295-300.
- Fernández-Miranda C, Paz M, Aranda JL, et al. Homocysteine and progression of carotid atherosclerosis in patients with coronary disease. Med Clin (Barc). 2003 Nov 1;121(15):561-4.
- Cacciapuoti F. Lowering homocysteine levels may prevent cardiovascular impairments? Possible therapeutic behaviors. Blood Coagul Fibrinolysis. 2012 Dec;23(8):677-9
- Liu MY, Hu DY. The predictive value of serum advanced fibrinogen and uric acid for acute coronary event risk. Zhonghua Yi Xue Za Zhi. 2006 Mar 14;86(10):678-80.
- Wattanakit K, Folsom AR, Chambless LE, Nieto FJ. Risk factors for cardiovascular event recurrence in the Atherosclerosis Risk in Communities (ARIC)study. Am Heart J. 2005 Apr;149(4):606-12.
- Maresca G, Di Blasio A, Marchioli R, Di Minno G. Measuring plasma fibrinogen to predict stroke and myocardial infarction: an update. Arterioscler Thromb Vasc Biol. 1999 Jun;19(6):1368-77.
- Acevedo M, Foody JM, Pearce GL, Sprecher DL. Fibrinogen: associations with cardiovascular events in an outpatient clinic. Am Heart J. 2002 Feb;143(2): 277-82.
- Drexel H, Amann FW, Beran J, et al. Plasma triglycerides and three lipoprotein cholesterol fractions are independent predictors of the extent of coronary atherosclerosis. Circulation. 1994 Nov;90(5):2230-5.
- Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007 Jul 18;298(3):309-16.
- Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007 Jul 18;298(3):299-308.
- Toikka JO, Ahotupa M, Viikari JS, et al. Constantly low HDL-cholesterol concentration relates to endothelial dysfunction and increased in vivo LDL-oxidation in healthy young men. Atherosclerosis. 1999 Nov 1;147(1):133-8.
- Viles-Gonzalez JF, Fuster V, Corti R, Badimon JJ. Emerging importance of HDL cholesterol in developing high-risk coronary plaques in acute coronary syndromes. Curr Opin Cardiol. 2003 Jul;18(4):286-94.
- Spieker LE, Sudano I, Hurlimann D, et al. High-density lipoprotein restores endothelial function in hypercholesterolemic men. Circulation. 2002 Mar 26;105(12):1399-402.
- Hak AE, Witteman JC, de Jong FH, Geerlings MI, Hofman A, Pols HA. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab. 2002 Aug;87(8):3632-9.
- English KM, Mandour O, Steeds RP, et al. Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J. 2000 Jun;21(11):890-4.
- Tivesten A, Mellström D, Jutberger H, et al. Low serum testosterone and high serum estradiol associate with lower extremity peripheral arterial disease in elderly men. The MrOS Study in Sweden. J Am Coll Cardiol. 2007 Sep 11;50(11):1070-6.
- Dunajska K, Milewicz A, Szymczak J, et al. Evaluation of sex hormone levels and some metabolic factors in men with coronary atherosclerosis. Aging Male. 2004 Sep;7(3):197-204.
- Phillips GB, Pinkernell BH, Jing TY. The association of hypotestosteronemia with coronary artery disease in men. Arterioscler Thromb. 1994 May;14(5):701-6.
- Jones RD, Nettleship JE, Kapoor D, Jones HT, Channer KS. Testosterone and atherosclerosis in aging men: purported association and clinical implications. Am J Cardiovasc Drugs. 2005;5(3): 141-54.
- Kiecolt-Glaser JK, Belury MA, Andridge R, Malarkey WB, Hwang BS, Glaser R. Omega-3 supplementation lowers inflammation in healthy middle-aged and older adults: a randomized controlled trial. Brain Behav Immun. 2012 Aug;26(6):988-95.
- Wu D, Han SN, Meydani M, Meydani SN. Effect of concomitant consumption of fish oil and vitamin E on production of inflammatory cytokines in healthy elderly humans. Ann NY Acad Sci. 2004 Dec;1031:422-4.
- Pischon T, Hankinson SE, Hotamisligil GS, et al. Habitual dietary intake of n-3 and n-6 fatty acids in relation to inflammatory markers among US men and women. Circulation. 2003 Jul 15;108(2):155-60.
- Mori TA, Beilin LJ. Omega-3 fatty acids and inflammation. Curr Atheroscler Rep. 2004 Nov;6(6):461-7.
- James MJ, Gibson RA, Cleland LG. Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr. 2000 Jan;71(1 Suppl): 343S-8S.
- Adam O, Beringer C, Kless T, et al. Anti-inflammatory effects of a low arachidonic acid diet and fish oil in patients with rheumatoid arthritis. Rheumatol Int. 2003 Jan;23(1):27-36.
- Lopez-Garcia E, Schulze MB, Manson JE, et al. Consumption of (n-3) fatty acids is related to plasma biomarkers of inflammation and endothelial activation in women. J Nutr. 2004 Jul;134(7): 1806-11.
- Lorenz R, Weber PC, Szimnau P, Heldwein W, Strasser T, Loeschke K. Supplementation with n-3 fatty acids from fish oil in chronic inflammatory bowel disease: A randomized, placebo-controlled, double-blind cross-over trial. J Intern Med Suppl. 1989;225(731): 225-32.
- Foitzik T, Eibl G, Schneider P, Wenger FA, Jacobi CA, Buhr HJ. Omega-3 fatty acid supplementation increases anti-inflammato ry cytokines and attenuates systemic disease sequelae in experimental pancreatitis. J Parenter Enteral Nutr. 2002 Nov-Dec;26(6):351-6.
- Nomura S, Kanazawa S, Fukuhara S. Effects of eicosapentaenoic acid on platelet activation markers and cell adhesion molecules in hyperlipidemic patients with Type 2 diabetes mellitus. J Diabetes Complications. 2003 May-Jun;17(3):153-9.
- Mori TA, Beilin LJ, Burke V, Morris J, Ritchie J. Interactions between dietary fat, fish, and fish oils and their effects on platelet function in men at risk of cardiovascular disease. Arterioscler Thromb Vasc Biol. 1997 Feb;17(2):279-86.
- Abeywardena MY, Head RJ. Longchain n-3 polyunsaturated fatty acids and blood vessel function. Cardiovasc Res. 2001 Dec;52(3):361-71.
- Thorngren M, Gustafson A. Effects of 11-week increases in dietary eicosapentaenoic acid on bleeding time, lipids, and platelet aggregation. Lancet. 1981 Nov 28;2(8257):1190-3.
- Vanschoonbeek K, Feijge MAH, Paquay M, et al. Variable hypocoagulant effect of fish oil intake in humans: modulation of fibrinogen level and thrombin generation. Arterioscler Thromb Vasc Biol. 2004 Sept;24(9):1734–40.

