Life Extension Magazine®
As baby boomers age past 65 years, record total numbers are afflicted with dementias that cause loss of mental faculties.
Alzheimer’s, Parkinson’s, and mild cognitive impairment are all associated with brain aging.
While these disorders have different causes, new studies reveal one factor that can contribute to them all—a high blood level of homocysteine.
Excess homocysteine has long been associated with poor cardiovascular health.
Recent research shows that by impeding brain blood flow and inflicting cell damage, homocysteine contributes to cognitive deficits and various forms of dementia.
The solution is simple.
Check homocysteine levels with a blood test.
If elevated, add more bio-active B-vitamins to your supplement program.1,2
Homocysteine and Degenerative Brain Aging

The link between high homocysteine blood levels and increased Alzheimer’s and vascular dementia risks was demonstrated 20 years ago.3,4
Since then, clinical studies continue to reveal that homocysteine contributes to degenerative brain aging.
In 2018, using two decades of data, a group of experts published an international Consensus Statement in the Journal of Alzheimer’s Disease. They concluded that elevated homocysteine is:
“…a modifiable risk factor for development of cognitive decline, dementia, and Alzheimer’s disease in older persons.”5
In other words, if we reduce high homocysteine, we’ll likely slow brain aging.
What You Need to Know
Fighting Back Against Brain Aging
- Homocysteine is an amino acid that is normally detoxified by processes that require vitamins B6, B12, B2 and folic acid to work. If there isn’t enough of those compounds, homocysteine can build up.
- High homocysteine is associated with accelerated brain aging and cardiovascular disease. Lowering homocysteine is a priority for disease prevention.
- Getting an annual blood test for homo-cysteine is vital, especially for those with family histories of dementia, heart disease and stroke.
- Preventing homocysteine buildup or lowering high levels can be accomplished by increasing intake of vitamin B6 (as pyridoxal 5’-phosphate), B12 (as methyl-cobalamin), folic acid (as 5-MTHF), and B2 (as riboflavin).
How Homocysteine Speeds Brain Aging
Homocysteine damages the brain via:6-13
Chronic inflammatory reactions,
Formation of atherosclerotic plaque that obstructs blood flow,
Shrinkage of brain areas like the hippocampus that are involved in memory formation,
Development of the neurofibrillary tangles and beta-amyloid plaque that trigger cell death, and
Hindrance of normal DNA repair needed for brain cell maintenance.
The link between high homocysteine and vascular dementia has been clear for several years.
Vascular dementia arises when blood vessels narrow, leading to diminished blood flow to vital brain areas.
Studies have shown that elevated homocysteine is associated with a 4.2-fold to 10.5-fold increased risk for vascular dementia.14,15
New studies published in 2019 also connect homocysteine levels to accelerated brain aging in Alzheimer’s and Parkinson’s diseases. Among their findings:
Alzheimer’s patients have elevated homocysteine levels that correlate with the degree of cognitive impairment. Higher homocysteine levels are associated with delusion, agitation/aggression, and depression.16
Parkinson’s disease patients with the highest homocysteine levels showed abnormal areas associated with poor brain blood flow.17
Homocysteine and Heart Disease

Back in 1981, Life Extension® urged readers to keep homocysteine levels low to protect against heart attack and stroke.
More than 38 years ago, researchers discovered that homocysteine was harmful to the endothelium, the lining of blood vessels throughout the body, impairing the endothelium’s ability to respond to changes in blood flow and pressure.18,19
These injuries accumulate, resulting in the development of inflammatory plaque that reduces, and eventually blocks, blood flow through the vessel. If that vessel is in the heart or brain, a catastrophic heart attack or stroke could occur.
High homocysteine has been identified as an independent risk factor associated with atherosclerosis and its consequences, raising the likelihood of vascular occlusion and sudden death.19,20
One study of more than 3,000 patients with chronic heart disease found that high homocysteine levels were associated with 2.5 times higher risk of coronary events. Each 5 µmol/L increase in homocysteine produced a 25% increase in risk.20
Other studies show that high homocysteine predicts poor outcomes in people who have survived a heart attack or had stents placed.21,22
Impaired endothelial function is especially risky in patients with diabetes, whose vessels already have a tendency to stiffen and form clots because of glucose-induced vessel damage.18
Poor endothelial function caused or worsened by high homocysteine leads to a host of other dangerous problems, including:
Reduced ability of the heart to create detours around a blocked vessel. This “collateral circulation” is vital in keeping the heart functioning as coronary arteries narrow.23
Reduced ability to counteract abnormal clotting inside an artery, which increases the risk of occlusive vascular events like ischemic stroke and acute heart attack.24
Increased arterial stiffness, a contributor to aortic stenosis, coronary artery disease, and ischemic stroke.25
Lowering Homocysteine Levels
Homocysteine is easily measured using low-cost blood tests.
Life Extension® advises homocysteine levels below 12 µmol/L, with ideal numbers being under 8 µmol/L.
Conventional reference ranges do not flag a homocysteine problem until blood levels reach 15 µmol/L. Published data reveal those with homo-cysteine blood levels between 10 µmol/L-15 µmol/L are at greater risk.26-28
The proper combination of low-cost B-vitamins supports two different homocysteine detoxification (removal) pathways in your body.
If your blood test result shows less-than-optimal levels, initiate a B-vitamin regimen based on the degree of homocysteine elevation. In the next column are some B-vitamin dosing suggestions.
American Heart Association Update March 18, 2019
 |
Homocysteine is a byproduct mostly related to ingesting an amino acid called methionine.
Those who eat a lot of red meat often have higher homocysteine blood levels that are attributed to the methionine content of red meat.
Homocysteine is detoxified in the body via two independent pathways as follows:
1. Methylation (dependent on folic acid, vitamin B12 and B2) and
2. Transsulfuration (dependent on vitamin B6)
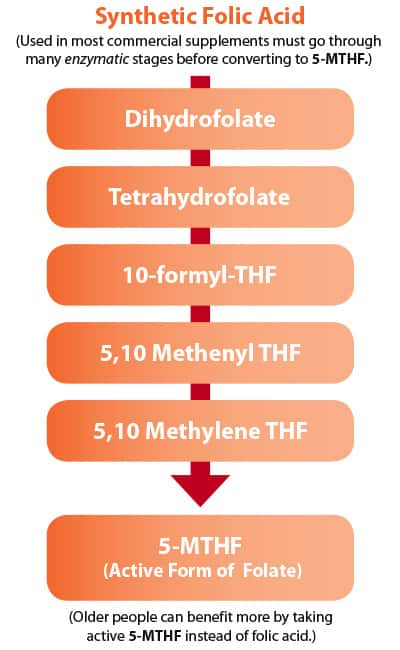
Young people readily convert B-vitamins into active forms that readily metabolize homocysteine.
As we age, however, enzymes in our body needed to transform B-vitamins into their active forms are lost. This is one reason why people who had low homocysteine levels in younger years see homocysteine surge higher as they grow older.
The solution to escalating homocysteine is supplementation with active forms of folic acid (5-MTHF), vitamin B6 (pyridoxal-5’ phosphate) and the neurologically- active form of B12 called methylcobalamin.
These forms of B-vitamins do not require enzymatic conversion in your body and are immediately available to detoxify homocysteine.
Homocysteine-Lowering Nutrients
Since B-vitamins are water soluble, those with stubbornly high homocysteine levels should take B-vitamin supplements twice daily. Here are daily B-vitamin supplement suggestions:
- Folic acid as activated 5-MTHF, 1,000 mcg to 10,000 mcg
- Vitamin B6 as activated pyridoxal 5’-phosphate, 100 mg to 200 mg
- Vitamin B12 as methylcobalamin, 300 mcg to 1,000 mcg
- Vitamin B2 as riboflavin, 25 mg to 100 mg
Retest your blood three months after initiating these supplements to ensure you are achieving optimal homocysteine levels.
Summary

Homocysteine is toxic and contributes to changes that increase risks of rapid brain aging and cardiovascular disorders.
Homocysteine tends to elevate with aging as detoxification systems in your body break down.
Low-cost B-vitamins can restore more youthful homocysteine detoxification via methylation and transsulfuration pathways in your body.
The ideal combination of B-vitamins turns on both these homocysteine removal pathways in your body.
Homocysteine can be lowered by increasing intake of: B6 (as pyridoxal 5’-phosphate), B12 (as methyl-cobalamin), folic acid (as 5-MTHF), and B2 (as riboflavin).
These vitamins help transform homocysteine into non-toxic compounds in your body.
For optimal protection against homocysteine buildup, have your blood tested.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Selhub J. Homocysteine metabolism. Annu Rev Nutr. 1999;19:217-46.
- Moat SJ, Ashfield-Watt PA, Powers HJ, et al. Effect of riboflavin status on the homocysteine-lowering effect of folate in relation to the MTHFR (C677T) genotype. Clin Chem. 2003 Feb;49(2):295-302.
- Clarke R, Smith AD, Jobst KA, et al. Folate, vitamin B12, and serum total homocysteine levels in confirmed Alzheimer disease. Arch Neurol. 1998 Nov;55(11):1449-55.
- McCaddon A, Davies G, Hudson P, et al. Total serum homocysteine in senile dementia of Alzheimer type. Int J Geriatr Psychiatry. 1998 Apr;13(4):235-9.
- Smith AD, Refsum H, Bottiglieri T, et al. Homocysteine and Dementia: An International Consensus Statement. J Alzheimers Dis. 2018;62(2):561-70.
- Papatheodorou L, Weiss N. Vascular oxidant stress and inflammation in hyperhomocysteinemia. Antioxid Redox Signal. 2007 Nov;9(11):1941-58.
- Weiss N, Keller C, Hoffmann U, et al. Endothelial dysfunction and atherothrombosis in mild hyperhomocysteinemia. Vasc Med. 2002 Aug;7(3):227-39.
- Tan B, Venketasubramanian N, Vrooman H, et al. Homocysteine and Cerebral Atrophy: The Epidemiology of Dementia in Singapore Study. J Alzheimers Dis. 2018;62(2):877-85.
- Kruman, II, Kumaravel TS, Lohani A, et al. Folic acid deficiency and homocysteine impair DNA repair in hippocampal neurons and sensitize them to amyloid toxicity in experimental models of Alzheimer’s disease. J Neurosci. 2002 Mar 1;22(5):1752-62.
- Li JG, Chu J, Barrero C, et al. Homocysteine exacerbates beta-amyloid pathology, tau pathology, and cognitive deficit in a mouse model of Alzheimer disease with plaques and tangles. Ann Neurol. 2014 Jun;75(6):851-63.
- Smith AD, Smith SM, de Jager CA, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PLoS One. 2010 Sep 8;5(9):e12244.
- Choe YM, Sohn BK, Choi HJ, et al. Association of homocysteine with hippocampal volume independent of cerebral amyloid and vascular burden. Neurobiol Aging. 2014 Jul;35(7):1519-25.
- Guthikonda S, Haynes WG. Homocysteine: role and implications in atherosclerosis. Curr Atheroscler Rep. 2006 Mar;8(2):100-6.
- Tan C, Peng W, Deng Y. Risk factors and predictive factors of cognitive deterioration in patients of vascular cognitive impairment no dementia with subcortical ischemic vascular disease. Zhonghua Yi Xue Za Zhi. 2014 Feb 11;94(5):352-5.
- Cervellati C, Romani A, Seripa D, et al. Oxidative balance, homocysteine, and uric acid levels in older patients with Late Onset Alzheimer’s Disease or Vascular Dementia. J Neurol Sci. 2014 Feb 15;337(1-2):156-61.
- Soni RM, Tiwari SC, Mahdi AA, et al. Serum Homocysteine and Behavioral and Psychological Symptoms of Dementia: Is There Any Correlation in Alzheimer’s Disease? Ann Neurosci. 2019 Jan;25(3):152-9.
- Shen Y, Dong ZF, Pan PL, et al. Association of homocysteine, folate, and white matter hyperintensities in Parkinson’s patients with different motor phenotypes. Neurol Sci. 2019 May 4.
- Doupis J, Eleftheriadou I, Kokkinos A, et al. Acute hyperhomocysteinemia impairs endothelium function in subjects with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2010 Jul;118(7):453-8.
- Lai WK, Kan MY. Homocysteine-Induced Endothelial Dysfunction. Ann Nutr Metab. 2015;67(1):1-12.
- Haim M, Tanne D, Goldbourt U, et al. Serum homocysteine and long-term risk of myocardial infarction and sudden death in patients with coronary heart disease. Cardiology. 2007;107(1):52-6.
- Yeh JK, Chen CC, Hsieh MJ, et al. Impact of Homocysteine Level on Long-term Cardiovascular Outcomes in Patients after Coronary Artery Stenting. J Atheroscler Thromb. 2017 Jul 1;24(7):696-705.
- Ma Y, Li L, Geng XB, et al. Correlation Between Hyperhomocysteinemia and Outcomes of Patients With Acute Myocardial Infarction. Am J Ther. 2016 Nov/Dec;23(6):e1464-e8.
- Nagai Y, Tasaki H, Miyamoto M, et al. Plasma level of homocysteine is inversely-associated with the development of collateral circulation in patients with single-vessel coronary artery disease. Circ J. 2002 Feb;66(2):158-62.
- Speidl WS, Nikfardjam M, Niessner A, et al. Mild hyperhomocysteinemia is associated with a decreased fibrinolytic activity in patients after ST-elevation myocardial infarction. Thromb Res. 2007;119(3):331-6.
- van Dijk SC, Smulders YM, Enneman AW, et al. Homocysteine level is associated with aortic stiffness in elderly: cross-sectional results from the B-PROOF study. J Hypertens.2013 May;31(5):952-9.
- Iso H, Moriyama Y, Sato S, et al. Serum total homocysteine concentrations and risk of stroke and its subtypes in Japanese. Circulation. 2004 Jun 08;109(22):2766-72.
- Nygard O, Nordrehaug JE, Refsum H, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997 Jul 24;337(4):230-6.
- Spence JD. Patients with atherosclerotic vascular disease: how low should plasma homocyst(e)ine levels go? Am J Cardiovasc Drugs. 2001;1(2):85-9.

